- Record: found
- Abstract: found
- Article: found
Log odds of positive lymph nodes is prognostically equivalent to lymph node ratio in non-metastatic colon cancer

Read this article at
Abstract
Background
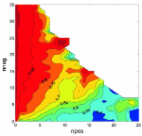
Globally, colorectal cancer (CRC) is the third and second leading cancer in men and women respectively with 600,000 deaths per year. Traditionally, clinicians have relied solely on nodal disease involvement, and measurements such as lymph node ratio (LNR; the ratio of metastatic/positive lymph nodes to total number of lymph nodes examined), when determining patient prognosis in CRC. The log odds of positive lymph nodes (LODDS) is a logistic transformation formula that uses pathologic lymph node data to stratify survival differences among patients within a single stage of disease. This formula allows clinicians to identify whether patients with clinically aggressive tumours fall into higher-risk groups regardless of nodal positivity and can potentially guide adjuvant treatment modalities. The aim of this study was to investigate whether LODDS in colon cancer provides better prognostication compared to LNR.
Methods
A retrospective study of patients on the prospectively maintained Cabrini Monash University Department of Surgery colorectal neoplasia database, incorporating data from hospitals in Melbourne Australia, identified patients entered between January 2010 and March 2016. Association of LODDS and LNR with clinical variables were analysed. Disease-free (DFS) and overall (OS) survival were investigated with Cox regression and Kaplan–Meier survival analyses.
Results
There were 862 treatment episodes identified in the database (402 male, 47%). The median patient age was 73 (range 22–100 years). There were 799 colonic cancers and 63 rectosigmoid cancers. The lymph node yield (LNY) was suboptimal (< 12) in 168 patients (19.5%) ( p = 0.05). The 5-year OS for the different LNR groups were 86, 91 and 61% ( p < 0.001) for LNR 0 (655 episodes), LNR 1 (128 episodes) and LNR 2 (78 episodes), respectively. For LODDS, they were 85, 91 and 61% ( p < 0.001) in LODDS 0 (569 episodes), LODDS 1 (217 episodes) and LODDS 2 (75 episodes) groups ( p < 0.001). Overall survival rates were comparable between the LNR and LODDS group and for LNY < 12 and stage III patients when each were sub-grouped by LODDS and LNR.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Prognostic value of the lymph node ratio in stage III colorectal cancer: a systematic review.
- Record: found
- Abstract: found
- Article: not found
The prognostic superiority of log odds of positive lymph nodes in stage III colon cancer.