- Record: found
- Abstract: found
- Article: found
Listening panel agreement and characteristics of lung sounds digitally recorded from children aged 1–59 months enrolled in the Pneumonia Etiology Research for Child Health (PERCH) case–control study
Read this article at
Abstract
Introduction
Paediatric lung sound recordings can be systematically assessed, but methodological feasibility and validity is unknown, especially from developing countries. We examined the performance of acoustically interpreting recorded paediatric lung sounds and compared sound characteristics between cases and controls.
Methods
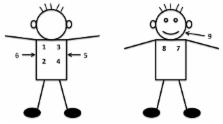
Pneumonia Etiology Research for Child Health staff in six African and Asian sites recorded lung sounds with a digital stethoscope in cases and controls. Cases aged 1–59 months had WHO severe or very severe pneumonia; age-matched community controls did not. A listening panel assigned examination results of normal, crackle, wheeze, crackle and wheeze or uninterpretable, with adjudication of discordant interpretations. Classifications were recategorised into any crackle, any wheeze or abnormal (any crackle or wheeze) and primary listener agreement (first two listeners) was analysed among interpretable examinations using the prevalence-adjusted, bias-adjusted kappa (PABAK). We examined predictors of disagreement with logistic regression and compared case and control lung sounds with descriptive statistics.
Results
Primary listeners considered 89.5% of 792 case and 92.4% of 301 control recordings interpretable. Among interpretable recordings, listeners agreed on the presence or absence of any abnormality in 74.9% (PABAK 0.50) of cases and 69.8% (PABAK 0.40) of controls, presence/absence of crackles in 70.6% (PABAK 0.41) of cases and 82.4% (PABAK 0.65) of controls and presence/absence of wheeze in 72.6% (PABAK 0.45) of cases and 73.8% (PABAK 0.48) of controls. Controls, tachypnoea, >3 uninterpretable chest positions, crying, upper airway noises and study site predicted listener disagreement. Among all interpretable examinations, 38.0% of cases and 84.9% of controls were normal (p<0.0001); wheezing was the most common sound (49.9%) in cases.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Respiratory risks from household air pollution in low and middle income countries.
- Record: found
- Abstract: found
- Article: not found
Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies.
- Record: found
- Abstract: found
- Article: not found