- Record: found
- Abstract: found
- Article: found
Diabetes mellitus is associated with increased mortality during tuberculosis treatment: a prospective cohort study among tuberculosis patients in South-Eastern Amahra Region, Ethiopia
Read this article at
Abstract
Background
There is growing evidence suggesting that diabetes mellitus (DM) affects disease presentation and treatment outcome in tuberculosis (TB) patients. This study aimed at investigating the role of DM on clinical presentations and treatment outcomes among newly diagnosed TB patients.
Methods
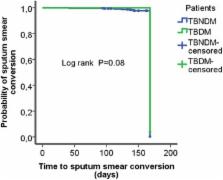
A prospective cohort study was conducted in South-Eastern Amhara Region, Ethiopia from September 2013 till March 2015. Study subjects were consecutively recruited from 44 randomly selected health facilities in the study area. Participants were categorized into two patient groups, namely, patients with TB and DM (TBDM) and TB patients without DM (TBNDM). Findings on clinical presentations and treatment outcomes were compared between the two patient groups. Cox proportional hazard regression analysis was applied to identify factors associated with death.
Results
Out of 1314 TB patients enrolled in the study, 109 (8.3 %) had coexisting DM. TBDM comorbidity [adjusted hazard ratio (AHR) 3.96; 95 % confidence interval (C.I.) (1.76–8.89)], and TB coinfection with human immunodeficiency virus (HIV) [AHR 2.59; 95 % C.I. (1.21–5.59)] were associated with increased death. TBDM and TBNDM patients did not show significant difference in clinical symptoms at baseline and during anti-TB treatment period. However, at the 2 nd month of treatment, TBDM patients were more symptomatic compared to patients in the TBNDM group.
Conclusions
The study showed that DM is associated with increased death during TB treatment. DM has no association with clinical presentation of TB except at the end of the intensive phase treatment. Routine screening of TB patients for DM is recommended for early diagnosis and treatment of patients with TBDM comorbidity.
Related collections
Most cited references25

- Record: found
- Abstract: found
- Article: found
The impact of diabetes on tuberculosis treatment outcomes: A systematic review
- Record: found
- Abstract: found
- Article: not found
Immune dysfunction in patients with diabetes mellitus (DM).
- Record: found
- Abstract: found
- Article: not found