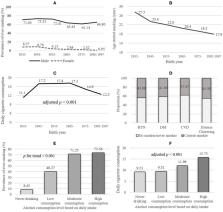
Excessive drinking is a significant cause of mortality, morbidity and social problems in many countries. Brief interventions aim to reduce alcohol consumption and related harm in hazardous and harmful drinkers who are not actively seeking help for alcohol problems. Interventions usually take the form of a conversation with a primary care provider and may include feedback on the person's alcohol use, information about potential harms and benefits of reducing intake, and advice on how to reduce consumption. Discussion informs the development of a personal plan to help reduce consumption. Brief interventions can also include behaviour change or motivationally‐focused counselling. This is an update of a Cochrane Review published in 2007. To assess the effectiveness of screening and brief alcohol intervention to reduce excessive alcohol consumption in hazardous or harmful drinkers in general practice or emergency care settings. We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and 12 other bibliographic databases to September 2017. We searched Alcohol and Alcohol Problems Science Database (to December 2003, after which the database was discontinued), trials registries, and websites. We carried out handsearching and checked reference lists of included studies and relevant reviews. We included randomised controlled trials (RCTs) of brief interventions to reduce hazardous or harmful alcohol consumption in people attending general practice, emergency care or other primary care settings for reasons other than alcohol treatment. The comparison group was no or minimal intervention, where a measure of alcohol consumption was reported. 'Brief intervention' was defined as a conversation comprising five or fewer sessions of brief advice or brief lifestyle counselling and a total duration of less than 60 minutes. Any more was considered an extended intervention. Digital interventions were not included in this review. We used standard methodological procedures expected by Cochrane. We carried out subgroup analyses where possible to investigate the impact of factors such as gender, age, setting (general practice versus emergency care), treatment exposure and baseline consumption. We included 69 studies that randomised a total of 33,642 participants. Of these, 42 studies were added for this update (24,057 participants). Most interventions were delivered in general practice (38 studies, 55%) or emergency care (27 studies, 39%) settings. Most studies (61 studies, 88%) compared brief intervention to minimal or no intervention. Extended interventions were compared with brief (4 studies, 6%), minimal or no intervention (7 studies, 10%). Few studies targeted particular age groups: adolescents or young adults (6 studies, 9%) and older adults (4 studies, 6%). Mean baseline alcohol consumption was 244 g/week (30.5 standard UK units) among the studies that reported these data. Main sources of bias were attrition and lack of provider or participant blinding. The primary meta‐analysis included 34 studies (15,197 participants) and provided moderate‐quality evidence that participants who received brief intervention consumed less alcohol than minimal or no intervention participants after one year (mean difference (MD) ‐20 g/week, 95% confidence interval (CI) ‐28 to ‐12). There was substantial heterogeneity among studies (I² = 73%). A subgroup analysis by gender demonstrated that both men and women reduced alcohol consumption after receiving a brief intervention. We found moderate‐quality evidence that brief alcohol interventions have little impact on frequency of binges per week (MD ‐0.08, 95% CI ‐0.14 to ‐0.02; 15 studies, 6946 participants); drinking days per week (MD ‐0.13, 95% CI ‐0.23 to ‐0.04; 11 studies, 5469 participants); or drinking intensity (‐0.2 g/drinking day, 95% CI ‐3.1 to 2.7; 10 studies, 3128 participants). We found moderate‐quality evidence of little difference in quantity of alcohol consumed when extended and no or minimal interventions were compared (‐20 g/week, 95% CI ‐40 to 1; 6 studies, 1296 participants). There was little difference in binges per week (‐0.08, 95% CI ‐0.28 to 0.12; 2 studies, 456 participants; moderate‐quality evidence) or difference in days drinking per week (‐0.45, 95% CI ‐0.81 to ‐0.09; 2 studies, 319 participants; moderate‐quality evidence). Extended versus no or minimal intervention provided little impact on drinking intensity (9 g/drinking day, 95% CI ‐26 to 9; 1 study, 158 participants; low‐quality evidence). Extended intervention had no greater impact than brief intervention on alcohol consumption, although findings were imprecise (MD 2 g/week, 95% CI ‐42 to 45; 3 studies, 552 participants; low‐quality evidence). Numbers of binges were not reported for this comparison, but one trial suggested a possible drop in days drinking per week (‐0.5, 95% CI ‐1.2 to 0.2; 147 participants; low‐quality evidence). Results from this trial also suggested very little impact on drinking intensity (‐1.7 g/drinking day, 95% CI ‐18.9 to 15.5; 147 participants; very low‐quality evidence). Only five studies reported adverse effects (very low‐quality evidence). No participants experienced any adverse effects in two studies; one study reported that the intervention increased binge drinking for women and two studies reported adverse events related to driving outcomes but concluded they were equivalent in both study arms. Sources of funding were reported by 67 studies (87%). With two exceptions, studies were funded by government institutes, research bodies or charitable foundations. One study was partly funded by a pharmaceutical company and a brewers association, another by a company developing diagnostic testing equipment. We found moderate‐quality evidence that brief interventions can reduce alcohol consumption in hazardous and harmful drinkers compared to minimal or no intervention. Longer counselling duration probably has little additional effect. Future studies should focus on identifying the components of interventions which are most closely associated with effectiveness. Effectiveness of brief alcohol interventions in primary care populations What is the aim of this review? We aimed to find out whether brief interventions with doctors and nurses in general practices or emergency care can reduce heavy drinking. We assessed the findings from 69 trials that involved a total of 33,642 participants; of these 34 studies (15,197 participants) provided data for the main analysis. Key messages Brief interventions in primary care settings aim to reduce heavy drinking compared to people who received usual care or brief written information. Longer interventions probably make little or no difference to heavy drinking compared to brief intervention. What was studied in the review? One way to reduce heavy drinking may be for doctors and nurses to provide brief advice or brief counselling to targeted people who consult general practitioners or other primary health care providers. People seeking primary healthcare are routinely asked about their drinking behaviour because alcohol use can affect many health conditions. Brief interventions typically include feedback on alcohol use and health‐related harms, identification of high risk situations for heavy drinking, simple advice about how to cut down drinking, strategies that can increase motivation to change drinking behaviour, and the development of a personal plan to reduce drinking. Brief interventions are designed to be delivered in regular consultations, which are often 5 to 15 minutes with doctors and around 20 to 30 minutes with nurses. Although short in duration, brief interventions can be delivered in one to five sessions. We did not include digital interventions in this review. Search date The evidence is current to September 2017. Study funding Funding sources were reported by 60 (87%) studies. Of these, 58 studies were funded by government institutes, research bodies or charitable foundations. One study was partly funded by a pharmaceutical company and a brewers association, another by a company developing diagnostic testing equipment. Nine studies did not report study funding sources. What are the main results of the review? We included 69 controlled trials conducted in many countries. Most studies were conducted in general practice and emergency care. Study participants received brief intervention or usual care or written information about alcohol (control group). The amount of alcohol people drank each week was reported by 34 trials (15,197 participants) at one‐year follow‐up and showed that people who received the brief intervention drank less than control group participants (moderate‐quality evidence). The reduction was around a pint of beer (475 mL) or a third of a bottle of wine (250 mL) less each week. Longer counselling probably provided little additional benefit compared to brief intervention or no intervention. One trial reported that the intervention adversely affected binge drinking for women, and two reported that no adverse effects resulted from receiving brief interventions. Most studies did not mention adverse effects. Quality of the evidence Findings may have been affected because participants and practitioners were often aware that brief interventions focused on alcohol. Furthermore, some participants could not be contacted at one‐year follow‐up to report drinking levels. Overall, evidence was assessed as mostly moderate‐quality. This means the reported effect size and direction is likely to be close to the true effect of these interventions.