- Record: found
- Abstract: found
- Article: found
Evaluation of the usefulness of red blood cell distribution width in critically ill pediatric patients
Read this article at
Abstract
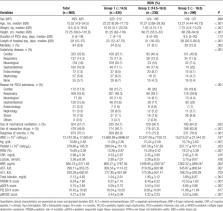
Red blood cell distribution width (RDW) is a component of routine complete blood count, which reflects variability in the size of circulating erythrocytes. Recently, there have been many reports about RDW as a strong prognostic marker in various disease conditions in the adult population. However, only a few studies have been performed in children. This study aimed to investigate the association between RDW and pediatric intensive care unit (PICU) mortality in critically ill children. This study includes 960 patients admitted to the PICU from November 2012 to May 2018. We evaluated the associations between RDW and clinical parameters including PICU mortality outcomes. The median age of the study population was 15.5 (interquartile range, 4.8–54.5) months. The mean RDW was 15.6% ± 3.3%. The overall PICU mortality was 8.8%. As we categorized patients into 3 groups with respect to RDW values (Group 1: ≤14.5%; Group 2: 14.5%–16.5%; and Group 3: >16.5%) and compared clinical parameters, the higher RDW groups (Groups 2 and 3) showed more use of vasoactive-inotropic drugs, mechanical ventilator support, higher severity scores, including pediatric risk of mortality III, pediatric sequential organ failure assessment, pediatric logistic organ dysfunction-2 (PELOD-2), and pediatric multiple organ dysfunction syndrome scores, and higher PICU mortality than the lower RDW group (Group 1) ( P < .05). Based on multivariate logistic regression analysis adjusted for age and sex, higher RDW value (≥14.5%) was an independent risk factor of PICU mortality. Moreover, adding RDW improved the performance of the PELOD-2 score in predicting PICU mortality (category-free net reclassification index 0.357, 95% confidence interval 0.153–0.562, P = .001). In conclusion, higher RDW value was significantly associated with worse clinical parameters including PICU mortality. RDW was an independent risk factor of PICU mortality and the addition of RDW significantly improved the performance of PELOD-2 score in predicting PICU mortality. Thus, RDW could be a promising prognostic factor with advantages of simple and easy measurement in critically ill pediatric patients.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Adaptation and Validation of a Pediatric Sequential Organ Failure Assessment Score and Evaluation of the Sepsis-3 Definitions in Critically Ill Children
- Record: found
- Abstract: found
- Article: not found
Red blood cell distribution width and mortality risk in a community-based prospective cohort.
- Record: found
- Abstract: found
- Article: not found