- Record: found
- Abstract: found
- Article: found
Differences between blood and cerebrospinal fluid glial fibrillary Acidic protein levels: The effect of sample stability
Read this article at
Abstract
Introduction
Recent evidence has shown that the marker of reactive astrogliosis, glial fibrillary acidic protein (GFAP), has a stronger relationship with cerebral amyloid beta (Aβ) pathology in blood than in cerebrospinal fluid (CSF). This study investigates if pre‐analytical treatment of blood and CSF contribute to these unexpected findings.
Methods
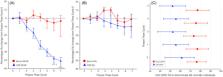
Paired CSF and serum samples from 49 individuals (Aβ‐negative = 28; Aβ‐positive = 21) underwent a series of seven freeze‐thaw cycles (FTCs). All samples were analyzed for GFAP and neurofilament light (NfL) using single molecule array technology including a fresh unfrozen sample from each patient.
Results
FTC significantly affected CSF GFAP concentration (−188.12 pg/ml per FTC) but not serum GFAP. In the same samples, NfL remained stable. Serum GFAP had a higher discrimination of Aβ burden than CSF GFAP, irrespective of FTC, which also included unfrozen samples.
Discussion
This study demonstrates large stability differences of GFAP in CSF and serum. However, this disparity does not seem to fully explain the stronger association of serum GFAP with Aβ pathology. Further work should investigate mechanisms of GFAP release into the bloodstream under pathological conditions.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: found
Discriminative Accuracy of Plasma Phospho-tau217 for Alzheimer Disease vs Other Neurodegenerative Disorders
- Record: found
- Abstract: found
- Article: not found
