- Record: found
- Abstract: found
- Article: found
Time trends in the prescription of statins for the primary prevention of cardiovascular disease in the United Kingdom: a cohort study using The Health Improvement Network primary care data
Abstract
Background
Statins are widely prescribed for the primary prevention of cardiovascular disease. Guidelines exist for statin prescriptions, but there is little recent analysis concerning prescription trends over time and how these vary with respect to demographic variables.
Methods and results
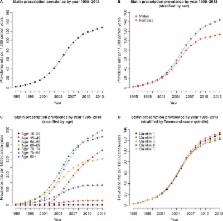
Using The Health Improvement Network primary care database, statin therapy initiation and statin prescription prevalence rates were calculated using data from 7,027,711 individuals across the UK for the years 1995 to 2013, overall and stratified by sex, age group, and socioeconomic deprivation level (Townsend score). Statin therapy initiation rates rose sharply from 1995 (0.51 per 1,000 person-years) up to 2006 (19.83 per 1,000 person-years) and thereafter declined (10.76 per 1,000 person-years in 2013). Males had higher initiation rates than females and individuals aged 60–85 years had higher initiation rates than younger or more elderly age groups. Initiation rates were slightly higher as social deprivation level increased, after accounting for age and sex. Prescription prevalence increased sharply from 1995 (2.36 per 1,000 person-years) to 2013 (128.03 per 1,000 person-years) with males generally having a higher prevalence rate, over time, than females. Prevalence rates over time were generally higher for older age groups but were similar with respect to social deprivation level.
Conclusion
The uptake of statins within UK primary care has increased greatly over time with statins being more commonly prescribed to older patients in general and, in recent years, males appear to have been prescribed statins at higher rates than females. After accounting for age and sex, the statin therapy initiation rate increases with the level of social deprivation.
Related collections
Most cited references53
- Record: found
- Abstract: found
- Article: not found
General cardiovascular risk profile for use in primary care: the Framingham Heart Study.
- Record: found
- Abstract: found
- Article: not found
Prediction of Coronary Heart Disease Using Risk Factor Categories
- Record: found
- Abstract: found
- Article: not found