- Record: found
- Abstract: found
- Article: found
A case of a rosette-forming glioneuronal tumor arising from the pons with disappearance of contrast enhancement
case-report

Fumine Tanaka , MD
a ,
Megumi Matsukawa , MD
a ,
Ryota Kogue , MD
a ,
Maki Umino , MD, PhD
a ,
Masayuki Maeda , MD, PhD
b
,
* ,
Katsunori Uchida , MD, PhD
c ,
Hiroshi Imai , MD, PhD
c ,
Toshio Matsubara , MD, PhD
d ,
Hajime Sakuma , MD, PhD
a
22 May 2019
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
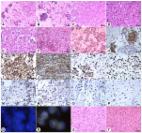
A rosette-forming glioneuronal tumor (RGNT) is a rare and slow-growing central nervous system tumor. This tumor is usually assessed by MRI during the follow-up period. RGNT can show alteration of contrast enhancement regardless of tumor growth. Here, we report a case of RGNT arising from pons which shows partial enhancement on initial MRI, smaller enhancement on follow-up MRI at 10 months, and totally disappeared at 18 months without any therapy.
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
A rosette-forming glioneuronal tumor of the fourth ventricle: infratentorial form of dysembryoplastic neuroepithelial tumor?
Takanori Hirose, B. Scheithauer, Takashi Komori (2002)
- Record: found
- Abstract: found
- Article: not found
Simple and complex dysembryoplastic neuroepithelial tumors (DNT) variants: clinical profile, MRI, and histopathology.
Pitt Niehusmann, Hans Clusmann, Paulo R A Campos … (2009)