- Record: found
- Abstract: found
- Article: found
Health Care Professionals’ Clinical Perspectives and Acceptance of a Blood Glucose Meter and Mobile App Featuring a Dynamic Color Range Indicator and Blood Sugar Mentor: Online Evaluation in Seven Countries
Abstract
Background
Despite many new therapies and technologies becoming available in the last decade, people with diabetes continue to struggle to achieve good glycemic control. Innovative and affordable solutions are needed to support health care professionals (HCPs) to improve patient outcomes.
Objective
To gather current self-management perceptions of HCPs in seven countries and investigate HCP satisfaction with a new glucose meter and mobile app featuring a dynamic color range indicator and a blood sugar mentor.
Methods
A total of 355 HCPs, including 142 endocrinologists (40.0%), 108 primary care physicians (30.4%), and 105 diabetes nurses (29.6%), were recruited from the United Kingdom (n=50), France (n=50), Germany (n=50), India (n=54), Algeria (50), Canada (n=51), and the United States (n=50). HCPs experienced the OneTouch Verio Reflect glucose meter and the OneTouch Reveal mobile app online from their own office computers using interactive demonstrations via webpages and multiple animations. After providing demographic and clinical practice insights, HCPs responded to statements about the utility of the system.
Results
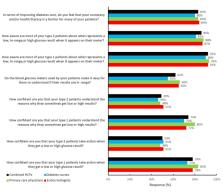
Concerning current practice, 83.1% (295/355) of HCPs agreed that poor numeracy or health literacy was a barrier for their patients. A total of 85.9% (305/355) and 92.1% (327/355) of HCPs responded that type 2 diabetes (T2D) and type 1 diabetes (T1D) patients were aware of what represented a low, in-range, or high blood glucose result. Only 62.0% (220/355) felt current glucose meters made it easy for patients to understand if results were in range. A total of 50.1% (178/355) and 78.0% (277/355) of HCPs were confident that T1D and T2D patients took action for low or high results. A total of 87.0% (309/355) agreed that the ColorSure Dynamic Range Indicator could help them teach patients how to interpret results and 88.7% (315/355) agreed it made them more aware of hyper- and hypoglycemic results so they could take action. A total of 83.7% (297/355) of HCPs agreed that the Blood Sugar Mentor feature gave personalized guidance, insight, and encouragement so patients could take action. A total of 82.8% (294/355) of HCPs also agreed that the Blood Sugar Mentor provided real-time guidance to reinforce the goals HCPs had set so patients could take steps to manage their diabetes between office visits. After experiencing the full system, 85.9% (305/355) of HCPs agreed it was beneficial for patients with lower numeracy or health literacy; 96.1% (341/355) agreed that it helped patients understand when results were low, in range, or high; and 91.0% (323/355) agreed that the way it displayed diabetes information would make patients more inclined to act upon results. A total of 89.0% (316/355) of HCPs agreed that it would be helpful for agreeing upon appropriate in-range goals for their patients for their next clinic visit.
Conclusions
This multi-country online study provides evidence that HCPs were highly satisfied with the OneTouch Verio Reflect meter and the OneTouch Reveal mobile app. Each of these use color-coded information and the Blood Sugar Mentor feature to assist patients with interpreting, analyzing, and acting upon their blood glucose results, which is particularly beneficial to keep patients on track between scheduled office visits.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Achievement of goals in U.S. diabetes care, 1999-2010.
- Record: found
- Abstract: found
- Article: not found
Association of numeracy and diabetes control.
- Record: found
- Abstract: found
- Article: not found