- Record: found
- Abstract: found
- Article: found
A phase 1, single-dose study of fresolimumab, an anti-TGF-β antibody, in treatment-resistant primary focal segmental glomerulosclerosis
Read this article at
Abstract
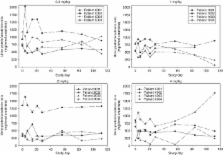
Primary focal segmental glomerulosclerosis (FSGS) is a disease with poor prognosis and high unmet therapeutic need. Here, we evaluated the safety and pharmacokinetics of single-dose infusions of fresolimumab, a human monoclonal antibody that inactivates all forms of transforming growth factor-β (TGF-β), in a phase I open-label, dose-ranging study. Patients with biopsy-confirmed, treatment-resistant, primary FSGS with a minimum estimated glomerular filtration rate (eGFR) of 25 ml/min per 1.73 m 2, and a urine protein to creatinine ratio over 1.8 mg/mg were eligible. All 16 patients completed the study in which each received one of four single-dose levels of fresolimumab (up to 4 mg/kg) and was followed for 112 days. Fresolimumab was well tolerated with pustular rash the only adverse event in two patients. One patient was diagnosed with a histologically confirmed primitive neuroectodermal tumor 2 years after fresolimumab treatment. Consistent with treatment-resistant FSGS, there was a slight decline in eGFR (median decline baseline to final of 5.85 ml/min per 1.73 m 2). Proteinuria fluctuated during the study with the median decline from baseline to final in urine protein to creatinine ratio of 1.2 mg/mg with all three Black patients having a mean decline of 3.6 mg/mg. The half-life of fresolimumab was ∼14 days, and the mean dose-normalized Cmax and area under the curve were independent of dose. Thus, single-dose fresolimumab was well tolerated in patients with primary resistant FSGS. Additional evaluation in a larger dose-ranging study is necessary.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
The Notch pathway in podocytes plays a role in the development of glomerular disease.
- Record: found
- Abstract: found
- Article: not found
Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data.
- Record: found
- Abstract: found
- Article: not found