- Record: found
- Abstract: found
- Article: found
Feasibility and Preliminary Effects of a Virtual Environment for Adults With Type 2 Diabetes: Pilot Study
Abstract
Background
Innovative interventions that empower patients in diabetes self-management (DSM) are needed to provide accessible, sustainable, cost-effective patient education and support that surpass current noninteractive interventions. Skills acquired in digital virtual environments (VEs) affect behaviors in the physical world. Some VEs are programmed as real-time three-dimensional representations of various settings via the Internet. For this research, a theoretically grounded VE that facilitates DSM was developed and pilot tested. It offered weekly synchronous DSM education classes, group meetings, and social networking in a community in which participants practiced real world skills such as grocery shopping, exercising, and dining out, allowing for interactive knowledge application. The VE was available 24/7 on the Internet, minimizing access barriers.
Objective
The objective of this study was to evaluate the feasibility and efficacy of participation in a VE for DSM education and support.
Methods
This study utilized a single group, pre-mid-post measure design. At 0, 3, and 6 months, we assessed participants’ perceived VE usability and usefulness, self-efficacy, diabetes self-management behaviors, perceived social support, and diabetes knowledge using validated survey measures; and we recorded metabolic indicators (HbA1c, BP, BMI). Process data were continuously collected in the VE (log-ins, voice recordings, locations visited, objects interacted with, and movement). Data analysis included descriptive statistics, t tests to evaluate changes in mediators and outcomes over time, and depiction of utilization and movement data.
Results
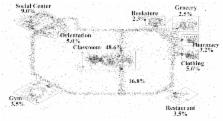
We enrolled 20 participants (13/20, 65% white, 7/20, 35% black), with an age range of 39-72 years (mean age, 54 years) and diabetes duration from 3 months to 25 years. At baseline, 95% (18/19) and 79% (15/19) of participants rated usefulness and ease of use as high on validated surveys with no significant changes at 3 or 6 months. Participants logged into the site a mean of 2.5 hours/week over the course of 6 months. High DSM class attendance was reflected by the largest percentage of time spent in the classroom (48.6%). Self-efficacy, social support, and foot care showed significant improvement ( P<.05). There were improvement trends in clinical outcomes that were clinically meaningful but did not reach statistical significance given the small sample size.
Conclusions
Because relatively little is known about usability, acceptability, and efficacy of health interventions in VEs, this study constitutes an important, innovative first step in exploring the potential of VEs for facilitating DSM. The preliminary data suggest that VEs provide a feasible and useful platform for patients and educators that affects self-management and related mediators. Flexible access to both synchronous and asynchronous diabetes education, skill building activities, and support from a home computer remove barriers to attending clinic-based meetings. This program has potential for improving DSM in an easily disseminated alternative model.
Related collections
Most cited references49
- Record: found
- Abstract: not found
- Article: not found
Crossing the Quality Chasm: A New Health System for the 21st Century
- Record: found
- Abstract: found
- Article: found
Sharing Health Data for Better Outcomes on PatientsLikeMe
- Record: found
- Abstract: found
- Article: not found