- Record: found
- Abstract: found
- Article: found
Effects of intravenous anesthesia with sevoflurane combined with propofol on intraoperative hemodynamics, postoperative stress disorder and cognitive function in elderly patients undergoing laparoscopic surgery
Read this article at
Abstract
Objectives:
To analyze the effects of intravenous anesthesia with sevoflurane combined with propofol on intraoperative hemodynamics, postoperative stress disorder and cognitive function in elderly patients undergoing laparoscopic surgery.
Methods:
Eighty elderly patients undergoing laparoscopic surgery in Xianning Central Hospital from September 2014 to February 2018. Enrolled patients were divided into observation group (n=40) and control group (n=40) according to the random regionalization method. Patients in the control group were given intravenous anesthesia with propofol, while those in the observation group were provided with a combined use of sevoflurane based on the method in the control group. The general surgical data, intraoperative hemodynamics, postoperative stress disorder and cognitive function were compared between the two groups.
Results:
There were no blood transfusions and no complications during operation in the two groups, and the operation completed successfully. There was no significant difference in the time of unconsciousness, intubation time, and duration of pneumoperitoneum establishment (p>0.05). However, the spontaneous breathing time, eye opening time upon calling and extubation time in observation group were shorter than those in control group (p<0.05). The heart rate (HR) in the two groups at intubation and at exploration was significantly higher than that at the time of entering the room (p<0.05), which was lower in observation group than that in control group (p<0.05). While there was no significant difference in the index at the other time points compared with that before entering the room and control group (p>0.05). The systolic blood pressure (SBP) had different degrees of change before intubation, after 0 minutes, three minutes and six minutes of intubation, after 0 minutes and five minutes of pneumoperitoneum establishment and at exploration when compared with that before entering the room (p<0.05). But the SBP at intubation and at exploration was significantly lower in observation group than that in control group (p<0.05). MAP was only decreased significantly at intubation compared with that before entering the room (p<0.05). At exploration, there was no significant fluctuation in the MAP level in observation group (p>0.05), but the MAP was increased significantly in control group (p<0.05). In addition, the postoperative stress disorder in observation group was milder than that in control group (p<0.05), and the postoperative cognitive function was better than that in control group (p<0.05).
Conclusions:
Intravenous anesthesia with sevoflurane combined with propofol has little effects on intraoperative hemodynamics and postoperative cognitive function in elderly patients undergoing laparoscopic surgery. Besides, it can obtain better recovery quality and have milder postoperative stress disorder than single use of propofol.
Related collections
Most cited references20

- Record: found
- Abstract: found
- Article: found
Clinical Pharmacokinetics and Pharmacodynamics of Propofol
- Record: found
- Abstract: found
- Article: found
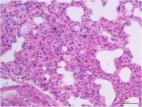
First report of Enterobacter hormaechei with respiratory disease in calves
- Record: found
- Abstract: found
- Article: not found
