- Record: found
- Abstract: found
- Article: found
Health conditions in adults with HIV compared with the general population: A population-based cross-sectional analysis
Read this article at
Summary
Background
Life expectancy in adults with human immunodeficiency virus (HIV) has increased and managing other health conditions is increasingly important for patients and healthcare planning. The aim of this study was to examine the prevalence and association between different health conditions and HIV status.
Methods
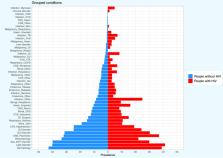
We performed a cross-sectional analysis of adult UK Clinical Practice Research Datalink primary care electronic medical records linked to hospital admissions as of Nov 30, 2015. We examined 47 health condition groups and 304 physical and mental health conditions by HIV status, after adjustment for age, sex, social deprivation status using logistic regression.
Findings
There were 964 patients with HIV (61.7% male; 92.8% aged <65 years) and 941,113 non-HIV patients (49.4% male; 75.2% aged <65 years). Condition groups with the greatest prevalence in HIV that were also highly prevalent in adults without HIV included: lipid disorder (41.4% vs 40.2%), and hypertension (19.1% vs 24.6%). Following adjustment, 18 (37.5%) condition groups were more likely in adults with HIV and ten (20.8%) were less likely. Individual conditions that were less likely in adults with HIV included: atrial fibrillation (odds ratio [OR] 0.37 [95% CI 0.20–0.64]) and hypertension (OR_0.78 [0.65–0.94]); rheumatoid arthritis (OR 0.27 [0.05–0.84]); asthma (OR_0.65 (0.53–0.80]); and certain eye diseases such as macular degeneration (OR_0.30 [0.09–0.70]). Meanwhile individual conditions that were more likely included: liver fibrosis, sclerosis, and cirrhosis (OR_3.23 [1.85–5.20]); pulmonary embolism (OR_2.06 [1.15–3.36]); male infertility (OR_2.23 [1.50–3.16]) and female infertility (OR_2.01 [1.34–2.88]); bipolar disorder (OR_2.93 [1.52–5.05]) and depression (OR_1.49 [1.28–1.71]); cervical malignancy (OR_4.64 [1.15–12.15]); and infections.
Related collections
Most cited references25
- Record: found
- Abstract: found
- Article: not found
Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study.

- Record: found
- Abstract: found
- Article: found
Data Resource Profile: Clinical Practice Research Datalink (CPRD)
- Record: found
- Abstract: found
- Article: not found