- Record: found
- Abstract: found
- Article: found
Percutaneous Cardiopulmonary Support-Supported Percutaneous Coronary Intervention: A Single Center Experience
Read this article at
Abstract
Background and Objectives
Percutaneous cardiopulmonary support (PCPS) has proven to be a valuable technique in high-risk coronary patients undergoing percutaneous coronary intervention (PCI). However, there have been few studies on PCI associated with PCPS in Korea. We summarized our experience with PCPS-supported PCI.
Subjects and Methods
We retrospectively reviewed 19 patients with PCPS-supported PCI between August 2005 and June 2009. PCPS was used as an elective procedure for 10 patients with at least two of the following conditions: left-ventricular ejection fraction <35%, target vessel(s) supplying more than 50% of the viable myocardium, high risk surgical patients, and patients who refused coronary bypass surgery. In the remaining 9 patients PCPS was used as an emergency procedure, to stabilize and even resuscitate patients with acute myocardial infarction and cardiogenic shock, in order to attempt urgent PCI.
Results
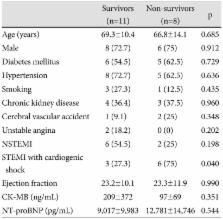
Among the 19 patients who were treated with PCPS-supported PCI, 11 (57.9%) survived and 8 (42.1%) patients did not. ST elevation myocardial infarction with cardiogenic shock was more prevalent in the non-survivors than in the survivors (75% vs. 27.3%, p=0.04). The elective PCPS-supported PCI was practiced more frequently in the survivors than in the non-survivors (72.7% vs. 25%, p=0.04). In the analysis of the event-free survival curve between elective and emergency procedures, there was a significant difference in the survival rate (p=0.025). Among the survivors there were more patients with multi-vessel disease, but a lower Thrombolysis in Myocardial Infarction grade in the culprit lesions was detected in the non-survivors, before PCI. Although we studied high-risk patients, there was no procedure-related mortality.
Related collections
Most cited references21
- Record: found
- Abstract: not found
- Article: not found
Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). Use of the Bramson membrane lung.
- Record: found
- Abstract: found
- Article: not found
Review of ECMO (extra corporeal membrane oxygenation) support in critically ill adult patients.
- Record: found
- Abstract: found
- Article: not found