- Record: found
- Abstract: found
- Article: found
The influence of aerobic fitness status on ventilatory efficiency in patients with coronary artery disease
Read this article at
Abstract
OBJECTIVE:
To test the hypotheses that 1) coronary artery disease patients with lower aerobic fitness exhibit a lower ventilatory efficiency and 2) coronary artery disease patients with lower initial aerobic fitness exhibit greater improvements in ventilatory efficiency with aerobic exercise training.
METHOD:
A total of 123 patients (61.0±0.7 years) with coronary artery disease were divided according to aerobic fitness status into 3 groups: group 1 (n = 34, peak VO 2<17.5 ml/kg/min), group 2 (n = 67, peak VO 2>17.5 and <24.5 ml/kg/min) and group 3 (n = 22, peak VO 2>24.5 ml/kg/min). All patients performed a cardiorespiratory exercise test on a treadmill. Ventilatory efficiency was determined by the lowest VE/VCO 2 ratio observed. The exercise training program comprised moderate-intensity aerobic exercise performed 3 times per week for 3 months. Clinicaltrials.gov: NCT02106533
RESULTS:
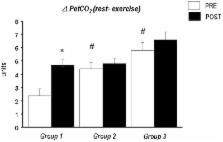
Before intervention, group 1 exhibited both lower peak VO 2 and lower ventilatory efficiency compared with the other 2 groups ( p<0.05). After the exercise training program, group 1 exhibited greater improvements in aerobic fitness and ventilatory efficiency compared with the 2 other groups (group 1: ▵ = -2.5±0.5 units; group 2: ▵ = -0.8±0.3 units; and group 3: ▵ = -1.4±0.6 units, respectively; p<0.05).
CONCLUSIONS:
Coronary artery disease patients with lower aerobic fitness status exhibited lower ventilatory efficiency during a graded exercise test. In addition, after 3 months of aerobic exercise training, only the patients with initially lower levels of aerobic fitness exhibited greater improvements in ventilatory efficiency.
Related collections
Most cited references68
- Record: found
- Abstract: found
- Article: not found
Exercise pathophysiology in patients with primary pulmonary hypertension.
- Record: found
- Abstract: found
- Article: not found
Ventilatory efficiency during exercise in healthy subjects.
- Record: found
- Abstract: found
- Article: not found