- Record: found
- Abstract: found
- Article: found
Comparison of Mean Platelet Volume, Platelet Count, Neutrophil/Lymphocyte Ratio and Platelet/Lymphocyte Ratio in the Euthyroid, Overt Hypothyroid and Subclinical Hyperthyroid Phases of Papillary Thyroid Carcinoma
Read this article at
Abstract
Introduction
Thyroid hormones are essential for the normal development, differentiation, metabolic balance and physiological function of all tissues. Mean platelet volume (MPV) indicates mean platelet size and reflects platelet production rate and stimulation. Increased platelet size has been observed in association with known cardiovascular risk factors. The neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR) are known markers of the systemic inflammatory response. This study aimed to investigate the effect of thyroid hormone changes by comparing platelet count, MPV values, NLR and PLR in thyroid papillary carcinoma.
Methods
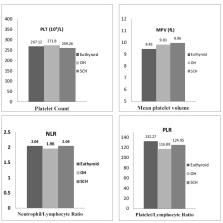
Forty-nine females and nine males comprising a total of 58 patients were included in the study. Clinical and laboratory parameters of patients were recorded in the following three phases of the disease: euthyroid phase (before thyroid surgery), overt hypothyroid (OH) phase (before radioactive iodine [RAI] treatment) and subclinical hyperthyroid (SCH) phase (six months after RAI treatment).
Results
The mean thyroid-stimulating hormone (TSH) values of the patients in the euthyroid, OH and SCH phases were 1.62±1.17, 76.4±37.5 and 0.09±0.07 µIU/mL, respectively. The mean MPV values of the patients in the euthyroid, OH and SCH phases were 9.45±1.33, 9.81±1.35 and 9.96±1.21 fL, respectively. MPV was significantly higher in the SCH phase than in the euthyroid phase (p=0.013). Platelet count, NLR and PLR were not statistically different between the euthyroid, OH and SCH phases.
Conclusion
The results of this study demonstrated that the levels of MPV increased significantly in the SCH phase in patients with papillary thyroid carcinoma (PTC), and increased MPV values contributed to increased risk of cardiovascular complications. These findings suggest that MPV can be a valuable, practical parameter for monitoring the haemostatic condition in thyroid disorders. No significant difference was observed in platelet count, NLR and PLR in all stages of PTC.
Related collections
Most cited references49
- Record: found
- Abstract: found
- Article: not found
Role of systemic inflammatory response in predicting survival in patients with primary operable cancer.
- Record: found
- Abstract: found
- Article: not found
Neutrophil to lymphocyte ratio and cardiovascular diseases: a review.
- Record: found
- Abstract: found
- Article: not found