- Record: found
- Abstract: found
- Article: found
Delivery of intravesical botulinum toxin A using low-energy shockwaves in the treatment of overactive bladder: A preliminary clinical study
Read this article at
ABSTRACT
Objective: To evaluate the efficacy and safety of botulinum toxin A (BoNT-A) instillation in the bladder under the effect of low-energy shockwaves (LESWs) for the treatment of refractory idiopathic overactive bladder (OAB).
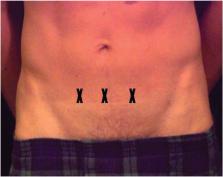
Patients and methods: A preliminary clinical study was conducted, including 15 patients with refractory OAB, between September 2016 and July 2017. Intravesical instillation of 100 IU of BoNT-A was done followed by LESWs (3000 shocks over 10 min) exposure to the supra-pubic area. Patients were followed-up by urine analysis, urine culture, post-void residual urine volume (PVR), and Overactive Bladder Symptom Score (OABSS) at 1, 2 and 3 months.
Results: There were statistically significant improvements in all OABSS domains and the total score after 1 and 2 months of treatment ( P < 0.05). Whereas, only the nocturia domain remained significantly improved after 3 months ( P = 0.02). There was no significant increase in PVR throughout the study period ( P > 0.05) and none of the patients required clean intermittent catheterisation. Two, two and three patients developed urinary tract infections after 1, 2 and 3 months, respectively.
Conclusion: Intravesical instillation of BoNT-A and LESWs is safe and effective method for the treatment of refractory OAB with a durable response for 2 months.
Abbreviations: BoNT-A: botulinum toxin A; CIC: clean intermittent catheterisation; DO: detrusor overactivity; LESWs: low-energy shockwaves; OAB: overactive bladder; OABSS: Overactive Bladder Symptom Score; Q max: maximum urinary flow rate; QoL: quality of life; UUI: urgency urinary incontinence
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Symptom assessment tool for overactive bladder syndrome--overactive bladder symptom score.
- Record: found
- Abstract: found
- Article: not found