- Record: found
- Abstract: found
- Article: found
National Survey Regarding the Management of Difficult Bile Duct Stones in South Korea
Read this article at
Abstract
Background/Aims
This study aimed to investigate the patterns of preferred endoscopic procedure types and techniques for managing difficult common bile duct (CBD) stones in South Korea.
Methods
The Committee of Policy and Quality Management of Korean Pancreatobiliary Association (KPBA) conducted a survey containing 19 questions. Both paper and online surveys were carried out; with the paper survey being conducted during the 2019 Annual Congress of KPBA and the online survey being conducted through Google Forms from April 2020 to February 2021.
Results
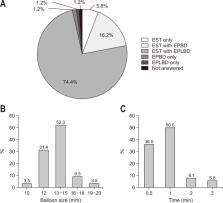
The response rate was approximately 41.3% (86/208). Sixty-two (73.0%) worked at tertiary hospitals or academic medical centers, and 60 (69.7%) had more than 5 years of endoscopic retrograde cholangiopancreatography experience. The preferred size criteria for large CBD stones were 15 mm (40.6%), 20 mm (31.3%), and 30 mm (4.6%). For managing of large CBD stones, endoscopic papillary large balloon dilation after endoscopic sphincterotomy was the most preferred technique (74.4%). When performing procedures in those with bleeding diathesis, 64 (74.4%) respondents favored endoscopic papillary balloon dilation (EPBD) alone or EPBD with small endoscopic sphincterotomy. Fifty-five respondents (63.9%) preferred the double-guidewire technique when faced with difficult bile duct cannulation in patients with periampullary diverticulum. In surgically altered anatomies, cap-fitted forward viewing endoscopy (76.7%) and percutaneous transhepatic cholangioscopy (48.8%) were the preferred techniques for Billroth-II anastomosis and total gastrectomy with Roux-en-Y anastomosis, respectively.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline
- Record: found
- Abstract: found
- Article: not found
Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline
- Record: found
- Abstract: not found
- Article: not found