- Record: found
- Abstract: found
- Article: found
Inspiratory effort impacts the accuracy of pulse pressure variations for fluid responsiveness prediction in mechanically ventilated patients with spontaneous breathing activity: a prospective cohort study
Read this article at
Abstract
Background
Pulse pressure variation (PPV) is unreliable in predicting fluid responsiveness (FR) in patients receiving mechanical ventilation with spontaneous breathing activity. Whether PPV can be valuable for predicting FR in patients with low inspiratory effort is unknown. We aimed to investigate whether PPV can be valuable in patients with low inspiratory effort.
Methods
This prospective study was conducted in an intensive care unit at a university hospital and included acute circulatory failure patients receiving volume-controlled ventilation with spontaneous breathing activity. Hemodynamic measurements were collected before and after a fluid challenge. The degree of inspiratory effort was assessed using airway occlusion pressure (P 0.1) and airway pressure swing during a whole breath occlusion (ΔP occ) before fluid challenge. Patients were classified as fluid responders if their cardiac output increased by ≥ 10%. Areas under receiver operating characteristic (AUROC) curves and gray zone approach were used to assess the predictive performance of PPV.
Results
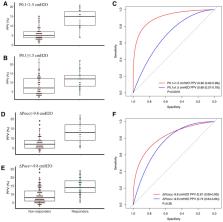
Among the 189 included patients, 53 (28.0%) were defined as responders. A PPV > 9.5% enabled to predict FR with an AUROC of 0.79 (0.67–0.83) in the whole population. The predictive performance of PPV differed significantly in groups stratified by the median value of P 0.1 (P 0.1 < 1.5 cmH 2O and P 0.1 ≥ 1.5 cmH 2O), but not in groups stratified by the median value of ΔP occ (ΔP occ < − 9.8 cmH 2O and ΔP occ ≥ − 9.8 cmH 2O). Specifically, in patients with P 0.1 < 1.5 cmH 2O, PPV was associated with an AUROC of 0.90 (0.82–0.99) compared with 0.68 (0.57–0.79) otherwise (p = 0.0016). The cut-off values of PPV were 10.5% and 9.5%, respectively. Besides, patients with P 0.1 < 1.5 cmH 2O had a narrow gray zone (10.5–11.5%) compared to patients with P 0.1 ≥ 1.5 cmH 2O (8.5–16.5%).
Conclusions
PPV is reliable in predicting FR in patients who received controlled ventilation with low spontaneous effort, defined as P 0.1 < 1.5 cmH 2O.
Trial registration NCT04802668. Registered 6 February 2021, https://clinicaltrials.gov/ct2/show/record/NCT04802668
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
A method of comparing the areas under receiver operating characteristic curves derived from the same cases.
- Record: found
- Abstract: found
- Article: not found
Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine
- Record: found
- Abstract: found
- Article: not found