- Record: found
- Abstract: found
- Article: found
Circulating Tumour Cells, Circulating Tumour DNA and Circulating MicroRNA in Metastatic Breast Carcinoma – What is the Role of Liquid Biopsy in Breast Cancer? Translated title: Zirkulierende Tumorzellen, zirkulierende Tumor-DNA und zirkulierende microRNA beim metastasierten Mammakarzinom – oder: Welche Rolle spielt die Liquid Biopsy beim Brustkrebs?
Read this article at
Abstract
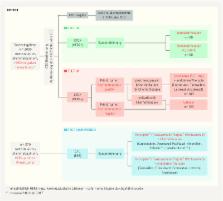
Dissemination of tumour cells and the development of solid metastases occurs via blood vessels and lymphatics. Circulating tumour cells (CTCs) and circulating tumour DNA (ctDNA) can be detected in venous blood in patients with early and metastatic breast cancer, and their prognostic relevance has been demonstrated on numerous occasions. Repeated testing for CTCs and ctDNA, or regular so-called “liquid biopsy”, can be performed easily at any stage during the course of disease. Additional molecular analysis allows definition of tumour characteristics and heterogeneity that may be associated with treatment resistance. This in turn makes personalised, targeted treatments possible that may achieve both improved overall survival and quality of life.
Zusammenfassung
Die Streuung von Tumorzellen und Entstehung solider Metastasen findet sowohl über das Lymph- als auch das Blutsystem statt. Der Nachweis zirkulierender Tumorzellen (CTCs) und der zirkulierenden Tumor-DNA (ctDNA) im venösen Blut ist sowohl beim frühen als auch beim metastasierten Mammakarzinom möglich. Ihre prognostische Relevanz wurde bereits mehrfach bewiesen. Dabei ist die repetitive Untersuchung der CTCs bzw. ctDNA im Sinne einer regelmäßigen „liquid biopsy“ jederzeit und problemlos möglich. Durch die zusätzlichen molekularen Analysen ist es möglich, Tumorcharakteristika und ihre Heterogenität, die mit möglichen Resistenzen einhergehen, zu definieren. Dies ermöglicht den Einsatz einer personalisierten und zielgerichteten Therapie, um neben einem verlängerten Gesamtüberleben auch die Verbesserung der Lebensqualität zu erreichen.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Circulating tumor cells and response to chemotherapy in metastatic breast cancer: SWOG S0500.

- Record: found
- Abstract: found
- Article: found
Circulating microRNAs as blood-based markers for patients with primary and metastatic breast cancer
- Record: found
- Abstract: found
- Article: not found