- Record: found
- Abstract: found
- Article: found
Strain Elastography Ultrasound: An Overview with Emphasis on Breast Cancer Diagnosis
Read this article at
Abstract
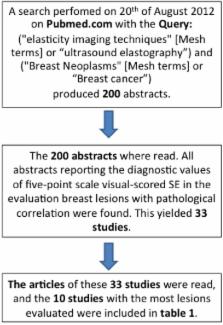
Strain elastography (SE), which estimates tissue strain, is an adjunct to the conventional ultrasound B-mode examination. We present a short introduction to SE and its clinical use. Furthermore, we present an overview of the 10 largest studies performed on the diagnostic accuracy of SE in breast cancer diagnostics. Eight of 10 studies presented data for both SE and B-mode imaging. Seven studies showed better specificity and accuracy for SE than for B-mode imaging in breast cancer diagnosis. Four studies showed an increase in specificity and accuracy when combining B-mode imaging with SE. The ways of combining B-mode imaging with SE in the diagnosis of breast cancer differed between the five studies. We believe that further studies are needed to establish an optimal algorithm for the combination of B-mode ultrasound and SE in breast cancer.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Elastography of breast lesions: initial clinical results.
- Record: found
- Abstract: found
- Article: not found
Interobserver agreement in assessing the sonographic and elastographic features of malignant thyroid nodules.
- Record: found
- Abstract: found
- Article: not found