- Record: found
- Abstract: found
- Article: found
Pénfigo vulgar con afectación exclusiva en el esófago: reporte de un caso Translated title: Pemphigus vulgaris with exclusive affectation in the esophagus: a case report
Read this article at
Resumen
Introducción:
el pénfigo vulgar comprende un grupo de enfermedades heterogéneas autoinmunes ampollosas de la piel y las mucosas. La afectación esofágica en el pénfigo vulgar es rara, con una prevalencia incierta que requiere un abordaje diagnóstico y terapéutico detallado.
Caso clínico:
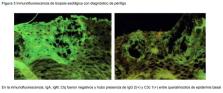
mujer de 37 años, con antecedentes de tratamiento con inhibidores de la Cox-2 debido a hernia discal. Se envió a Gastroenterología por pérdida de peso de aprox. 5 kg en un mes. La paciente tuvo presencia de disfagia, odinofagia y dolor retroesternal con pobre tolerancia a la vía oral. Se hizo endoscopía que reportó esofagitis disecante superficial y gastropatía eritematosa de antro; el duodeno estaba en estado normal. Los hallazgos se correlacionaron con el diagnóstico de pénfigo vulgar con afectación exclusiva a esófago. En la valoración no se identificaron lesiones en piel, cavidad oral u otras mucosas. Se hizo nueva endoscopía como control y se encontró inmunofluorescencia de biopsia esofágica reactiva a IgG 2. Se dio manejo inicial con glucocorticoides, antiinflamatorios e inmunosupresores.
Conclusiones:
la importancia del estudio del pénfigo radica no solo en la alta morbimortalidad asociada, sino en lo raro y complejo de su detección, pues los pacientes suelen tardar varios meses en tener un diagnóstico certero y aún más en conseguir las metas terapéuticas. Es prioritaria la difusión del estudio del pénfigo entre los profesionales de la salud involucrados en su detección.
Abstract
Pemphigus vulgaris comprises a group of heterogeneous blistering autoimmune diseases of the skin and mucosa. Esophageal involvement within pemphigus vulgaris is rare with an uncertain prevalence that requires a detailed diagnostic and a therapeutic approach.
37-year-old female, with a history of treatment with Cox-2 inhibitors due to herniated disc. She is sent to the Gastroenterology Service for weight loss of approximately 5 kilos in a month, with the presence of dysphagia, odynophagia and retrosternal pain with poor tolerance to the oral route. Endoscopy was performed, which reported esophagitis dissecans superficialis (EDS), erythematous gastropathy of the antrum and normal duodenum. Findings were correlated with the diagnosis of pemphigus vulgaris with exclusive involvement of the esophagus. The evaluation did not identify lesions on the skin, oral cavity or other mucous membranes. A new endoscopy was performed as a control and it was found immunofluorescence of the esophageal biopsy reactive to IgG 2. Initial management was given with glucocorticoids, anti-inflammatories and immunosuppressants.
The importance of the study of pemphigus lies not only in the high associated morbidity and mortality, but also in its intrinsic rarity and the complexity of its detection, given that patients usually take several months to have an accurate diagnosis and even more time to achieve therapeutic goals. It is a priority the dissemination of the study of pemphigus among health professionals involved in its detection.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Diagnosis and Management of Pemphigus: recommendations by an International Panel of Experts
- Record: found
- Abstract: found
- Article: not found
Autoimmunity to desmocollin 3 in pemphigus vulgaris.
- Record: found
- Abstract: found
- Article: not found
Esophagitis dissecans superficialis ("sloughing esophagitis"): a clinicopathologic study of 12 cases.
Author and article information
Comments
Comment on this article
Similar content258
- Evidências do cuidar de pessoas com pênfigo vulgar: desafio à enfermagem Translated title: Evidences related to the care of people with pemphigus vulgaris: a challenge to nursing Translated title: Evidencias del cuidar de personas con pénfigo vulgar: desafio a la enfermeríaAuthors: Euzeli da Silva Brandão, Iraci dos Santos