- Record: found
- Abstract: found
- Article: found
Hyposecretion of the Adrenal Androgen Dehydroepiandrosterone Sulfate (DHEA-S) in the Majority of the Alopecia Areata Patients: Is it a Primitive and Pathogenic Perturbation of Hypothalamic-Pituitary-Adrenal Axis?
letter
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Sir,
Basic and clinical research suggest that disturbed neuro-endocrine function may be
involved in the pathogenesis and course of autoimmune diseases. Hormones, such as
those of hypothalamic-pituitary-adrenal Axis (HPA), are known to operate a modulation
of immune responses.[1] In this report, we looked into the basal serum levels of four
hormones: prolactin, ACTH, cortisol, dehydroepiandrosterone sulfate (the stable metabolite
of the active steroid DHEA) by means of RIA method, to investigate if it could be
a gross HPA axis perturbation in severe cases of alopecia areata disease (involvement
>25% of scalp hair) as it appears in other autoimmune illness, such as in rheumatoid
arthritis, systemic lupus erythematosus, Sjogren disease[2] and Hashimoto's thyroiditis[3]
the last one so often associated to alopecia areata.[4] We studied a total of 142
patients - 55 males and 87 females- average age 34 years, not in systemic steroid
therapy [Table 1]; they are members of the “Associazione Mediterranea Alopecia Areata”
(www.alopecia-italy.com). We confirmed the normal value of prolactin level[5] and
did not find significant imbalance of basal level of ACTH and cortisol, but DHEA-S
in the majority of the patients was found reduced in comparison to age and sex matched
controls: 69.1% of males (M) and 74.7% of females (F) are below the media of the control
values – 165.80±98.69 mcg/dl (M) and 101.36±97.22 mcg /dl (F) versus 228.07±151.81
mcg/dl (M- control) and 134.49±104.64 mcg/dl (F -control) - Student's t-test P<0.00002
and Mood's median-test P<0.0000001 respectively-. 63.6% of M and 64.4% of F are in
the range of deficiency values - given by mean minus s.d./3: <177, 47 mcg/dl for M
and <99,60 mcg /dl for F [Figure 1]- irrespective of their age, clinical forms and
duration of the disease. At the moment, we cannot determine with certainty whether
this deficit is pre-existing or subsequent to the onset of pathology, but the low
DHEA-S secretion also found in the majority of the patients in the remission phase
and those with recent onset of the pathology -whereas cortisol and ACTH were in the
normal range- could be indicative of a primitive deficit of DHEA-S production. These
results confirm the old data from Vinocurow[6] and Montagnani:[7] they found in 85%
of patients a hypoadrenalism through dosing of urinary steroids, independently from
the clinical form of Alopecia. Many studies have shown that DHEA/DHEA-S has significant
immunomodulating activity and could be useful in restoring immune regulation in patients
with chronic autoimmune diseases,[8] probably through its capacity to modulate the
mechanisms of natural immunity, such as NK cells, that can control the activation
of T autoreactive linphocytes, event that appears in some autoimmune diseases, including
alopecia areata.[9] On the other hand, DHEA is a neurohormone with antidepressive
- ansiolytic activity and low DHEA-S secretion is considered as indicative of chronic
stress response,[10] whose involvement in the pathogenesis of AA is to be considered.[11]
Our preliminary therapeutic data suggest the clinical usefulness in some patients
of the normalitation of the defective level of DHEA-S, but it is mandatory to investigate
in a consistent number of cases affected from severe chronic/relapsing AA if the administration
of DHEA could be a new additive relatively safe and inexpensive resource for the stabilization
of this desperating disease, as it is suggested for other autoimmune pathologies.[8]
Table 1
Case study
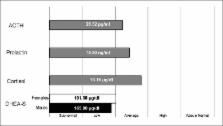
Figure 1
DHEA-S mean values in sample (normal mean and median: males=228.07±151.81 mcg/dl;
females=134.49±104.64 mcg/dl): Sample mean: males=165.80±98.69 mcg/dl (n=55, Student's
t-test P<0.00002), females=101.36±97.22 mcg/dl (n=87, not normally distributed, therefore,
given the median=73.8, Mood's median-test P<0.0000001).
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
Dehydroepiandrosterone as a regulator of immune cell function.
Jon Hazeldine, Wiebke Arlt, Janet M Lord (2010)
- Record: found
- Abstract: found
- Article: not found
Neural immune pathways and their connection to inflammatory diseases
- Record: found
- Abstract: found
- Article: not found
Low serum levels of sex steroids are associated with disease characteristics in primary Sjogren's syndrome; supplementation with dehydroepiandrosterone restores the concentrations.
Claes Ohlsson, Yrjö Konttinen, Fernand Labrie … (2009)