- Record: found
- Abstract: found
- Article: found
Myelodysplastic syndromes: advantages of a combined cytogenetic and molecular diagnostic workup
Read this article at
Abstract
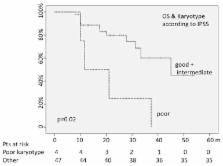
In this study we present a new diagnostic workup for the myelodysplastic syndromes (MDS) including FISH, aCGH, and somatic mutation assays in addition to the conventional cytogenetics (CC). We analyzed 61 patients by CC, FISH for chromosome 5, 7, 8 and PDGFR rearrangements, aCGH, and PCR for ASXL1, EZH2, TP53, TET2, RUNX1, DNMT3A, SF3B1 somatic mutations. Moreover, we quantified WT1 and RPS14 gene expression levels, in order to find their possible adjunctive value and their possible clinical impact. CC analysis showed 32% of patients with at least one aberration. FISH analysis detected chromosomal aberrations in 24% of patients and recovered 5 cases (13.5%) at normal karyotype (two 5q- syndromes, one del(7) case, two cases with PDGFR rearrangement). The aGCH detected 10 “new” unbalanced cases in respect of the CC, including one with alteration of the ETV6 gene. After mutational analysis, 33 patients (54%) presented at least one mutation and represented the only marker of clonality in 36% of all patients. The statistical analysis confirmed the prognostic role of CC either on overall or on progression-free-survival. In addition, deletions detected by aCGH and WT1 over-expression negatively conditioned survival. In conclusion, our work showed that 1) the addition of FISH (at least for chr. 5 and 7) can improve the definition of the risk score; 2) mutational analysis, especially for the TP53 and SF3B1, could better define the type of MDS and represent a “clinical warning”; 3) the aCGH use could be probably applied to selected cases (with suboptimal response or failure).
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
Revised international prognostic scoring system for myelodysplastic syndromes.
- Record: found
- Abstract: found
- Article: not found
Prognostic relevance of integrated genetic profiling in acute myeloid leukemia.
- Record: found
- Abstract: found
- Article: not found