- Record: found
- Abstract: found
- Article: found
The Prognostic Value of Residual Volume/Total Lung Capacity in Patients with Chronic Obstructive Pulmonary Disease

Read this article at
Abstract
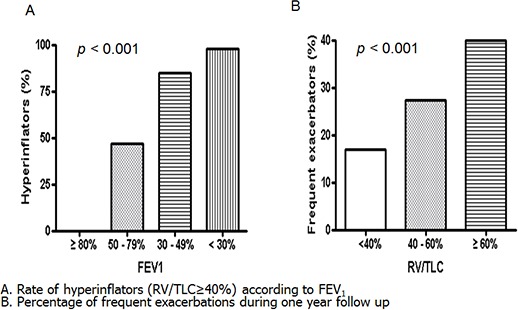
The prognostic role of resting pulmonary hyperinflation as measured by residual volume (RV)/total lung capacity (TLC) in chronic obstructive pulmonary disease (COPD) remains poorly understood. Therefore, this study aimed to identify the factors related to resting pulmonary hyperinflation in COPD and to determine whether resting pulmonary hyperinflation is a prognostic factor in COPD. In total, 353 patients with COPD in the Korean Obstructive Lung Disease cohort recruited from 16 hospitals were enrolled. Resting pulmonary hyperinflation was defined as RV/TLC ≥ 40%. Multivariate logistic regression analysis demonstrated that older age ( P = 0.001), lower forced expiratory volume in 1 second (FEV 1) ( P < 0.001), higher St. George Respiratory Questionnaire (SGRQ) score ( P = 0.019), and higher emphysema index ( P = 0.010) were associated independently with resting hyperinflation. Multivariate Cox regression model that included age, gender, dyspnea scale, SGRQ, RV/TLC, and 6-min walking distance revealed that an older age (HR = 1.07, P = 0.027), a higher RV/TLC (HR = 1.04, P = 0.025), and a shorter 6-min walking distance (HR = 0.99, P < 0.001) were independent predictors of all-cause mortality. Our data showed that older age, higher emphysema index, higher SGRQ score, and lower FEV 1 were associated independently with resting pulmonary hyperinflation in COPD. RV/TLC is an independent risk factor for all-cause mortality in COPD.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Susceptibility to exacerbation in chronic obstructive pulmonary disease.
- Record: found
- Abstract: found
- Article: not found
Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function.
- Record: found
- Abstract: found
- Article: not found