- Record: found
- Abstract: found
- Article: found
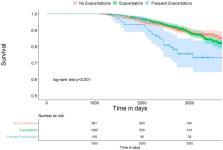
Increased mortality associated with frequent exacerbations in COPD patients with mild-to-moderate lung function impairment, and smokers with normal spirometry
Read this article at
Abstract
Background:
The burden of frequent respiratory exacerbations in COPD patients with mild-to-moderate spirometric impairment and smokers with preserved lung function is unknown.
Methods:
We categorized COPD participants in COPDGene with post-bronchodilator FEV1%predicted≥50% by the annual exacerbation frequency into three groups: i)frequent exacerbators (top 5%; n = 109), ii)exacerbators (>0 but less than frequent exacerbators; n = 1,009), and iii)No exacerbation (n = 981). Exacerbations were defined as respiratory episodes requiring antibiotics and/or systemic steroids. We performed a Cox proportional hazards regression analysis to examine the association with mortality. We repeated the same process in current/former smokers with preserved spirometry (FEV1≥80%predicted and FEV1/FVC≥0.7).
Results:
Among 2,099 COPD participants, frequent exacerbators had ≥1.8 exacerbations/year and were responsible for 34.3% of the total exacerbations. There were 102 (10.4%) deaths in the group with no exacerbations, 119 (11.8%) in the exacerbator group, and 24 (22%) in the frequent exacerbators. Adjusted mortality in frequent exacerbators was higher relative to individuals with no exacerbations (hazard ratio (HR) = 1.98; 95%CI = 1.25–3.13). An increase in frequency of exacerbations by one exacerbation/year was associated with increased mortality (HR = 1.40,95%CI = 1.21–1.62). Among 3,143 participants with preserved spirometry, frequent exacerbators had ≥0.8 exacerbations/year and were responsible for more than half of the exacerbations. There were 93 (4.2%) deaths in the group with no exacerbations, 28 (3.8%) in the exacerbator group, and 14 (7.6%) in the frequent exacerbators. The adjusted mortality was increased in frequent exacerbators with preserved spirometry relative to those with no exacerbations (HR = 2.25; 95%CI = 1.26–4.01).
Related collections
Most cited references39
- Record: found
- Abstract: not found
- Article: not found
Standardisation of spirometry.
- Record: found
- Abstract: found
- Article: not found
Susceptibility to exacerbation in chronic obstructive pulmonary disease.
- Record: found
- Abstract: not found
- Article: not found