- Record: found
- Abstract: found
- Article: found
Determinants of Maternal Insulin Resistance during Pregnancy: An Updated Overview
Read this article at
Abstract
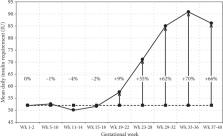
Insulin resistance changes over time during pregnancy, and in the last half of the pregnancy, insulin resistance increases considerably and can become severe, especially in women with gestational diabetes and type 2 diabetes. Numerous factors such as placental hormones, obesity, inactivity, an unhealthy diet, and genetic and epigenetic contributions influence insulin resistance in pregnancy, but the causal mechanisms are complex and still not completely elucidated. In this review, we strive to give an overview of the many components that have been ascribed to contribute to the insulin resistance in pregnancy. Knowledge about the causes and consequences of insulin resistance is of extreme importance in order to establish the best possible treatment during pregnancy as severe insulin resistance can result in metabolic dysfunction in both mother and offspring on a short as well as long-term basis.
Related collections
Most cited references55
- Record: found
- Abstract: found
- Article: not found
Fetal and infant growth and impaired glucose tolerance at age 64.
- Record: found
- Abstract: not found
- Article: not found
Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes.

- Record: found
- Abstract: found
- Article: found