- Record: found
- Abstract: found
- Article: found
The Northern Manhattan Caregiver Intervention Project: a randomised trial testing the effectiveness of a dementia caregiver intervention in Hispanics in New York City
Read this article at
Abstract
Objectives
Dementia prevalence and its burden on families are increasing. Caregivers of persons with dementia have more depression and stress than the general population. Several interventions have proven efficacy in decreasing depression and stress in selected populations of caregivers. Hispanics in New York City tend to have a higher burden of dementia caregiving compared to non-Hispanic whites (NHW) because Hispanics have a higher prevalence of dementia, tend to have high family involvement, and tend to have higher psychosocial and economic stressors. Thus, we chose to test the effectiveness of a dementia caregiving intervention, the New York University Caregiver Intervention (NYUCI), with demonstrated efficacy in spouse caregivers in Hispanic relative caregivers of persons with dementia. Including the community health worker (CHW) intervention in both arms alleviates general psychosocial stressors and allows the assessment of the effectiveness of the intervention. Compared to two original efficacy studies of the NYUCI, which included only spouse caregivers, our study includes all relative caregivers, including common law spouses, children, siblings, a nephew and nieces. This study will be the first randomised trial to test the effectiveness of the NYUCI in Hispanic caregivers including non-spouses.
Methods and analysis
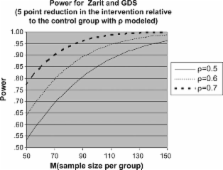
The design of the study is a randomised controlled trial (RCT). Participants are randomised to two arms: case management by a CHW and an intervention arm including the NYUCI in addition to case management by the CHW. The duration of intervention is 6 months. The main outcomes in the trial are changes in the Geriatric Depression Scale (GDS) and the Zarit Caregiver Burden Scale (ZCBS) from baseline to 6 months.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Book: not found
Statistical Power Analysis for the Behavioral Sciences
- Record: found
- Abstract: found
- Article: not found
Development and validation of a geriatric depression screening scale: a preliminary report.
- Record: found
- Abstract: found
- Article: not found