- Record: found
- Abstract: found
- Article: found
Clinical Management of Neuropsychiatric Symptoms of Huntington Disease: Expert-Based Consensus Guidelines on Agitation, Anxiety, Apathy, Psychosis and Sleep Disorders
Read this article at
Abstract
Background:
In clinical practice, several strategies and pharmacological options are available to treat neuropsychiatric symptoms of Huntington disease (HD). However, there is currently insufficient data for evidence-based guidelines on the management of these common symptoms.
Objective:
We aimed to develop expert-based recommendations regarding the management of agitation, anxiety, apathy, psychosis, and sleep disorders.
Methods:
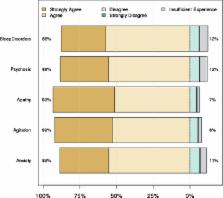
Guideline development was based on a modified Institute of Medicine guideline process that accounted for a lack of evidence base. An international committee of 11 multidisciplinary experts proposed a series of statements regarding the description and management of each symptom. Statement assessment and validation was performed using a web-based survey tool and 84 international HD experts (neurologists and psychiatrists) who assessed the statements and indicated their level of agreement.
Results:
High-level agreement (≥85% experts strongly agreed or agreed) was reached for 107 of the 110 statements that have been incorporated into the expert-based clinical recommendations presented herein.
Conclusions:
Clinical statements to guide the routine management of agitation, anxiety, apathy, psychosis, and sleep disorders in HD have been developed. Although not specifically tested in the HD population, clinical experience has shown that most of the neuropsychiatric symptoms discussed, when considered in isolation are treatable using pharmacologic and non-pharmacologic strategies developed for use in other populations. However, the management of neuropsychiatric symptoms in HD can be complex because neuropsychiatric symptoms often co-exist and treatment decisions should be adapted to cover all symptoms while limiting polypharmacy.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Neuropsychiatric aspects of Huntington's disease.
- Record: found
- Abstract: found
- Article: not found
Practice Parameter: evaluation and treatment of depression, psychosis, and dementia in Parkinson disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology.
- Record: found
- Abstract: found
- Article: not found