- Record: found
- Abstract: found
- Article: found
Modified Split-Scan Computed Tomography (CT) Diagnostics of Severely Injured Patients: First Results from a Level I Trauma Center Using a Dedicated Head-and-Neck CT-Angiogram for the Detection of Cervical Artery Dissections
Read this article at
Abstract
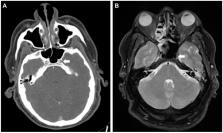
Introduction: Traumatic cervical artery dissections are associated with high mortality and morbidity in severely injured patients. After finding even higher incidences than reported before, we decided to incorporate a dedicated head-and-neck computed tomography angiogram (CT-A) in our imaging routine for patients who have been obviously severely injured or, according to trauma mechanism, are suspected to be severely injured. Materials and Methods: A total of 134 consecutive trauma patients with an ISS ≥ 16 admitted to our level I trauma center during an 18 month period were included. All underwent standardized whole-body CT in a 256-detector row scanner with a dedicated head-and-neck CT-A realized as single-bolus split-scan routine. Incidence, mortality, patient and trauma characteristics, and concomitant injuries were recorded and analyzed in patients with carotid artery dissection (CAD) and vertebral artery dissection (VAD). Results: Of the 134 patients included, 7 patients had at least one cervical artery dissection (CeAD; 5.2%; 95% CI 1.5–9.0%). Six patients (85.7%) had carotid artery dissections, with one patient having a CAD of both sides and one patient having a CAD and contralateral VAD combined. Two patients (28.6%) showed a VAD. Overall mortality was 14.3%, neurologic morbidity was 28.6%. None of the patients showed any attributable neurologic symptoms on admission. The new scanning protocol led to further 5 patients with suspected CeAD during the study period, all ruled out by additional magnetic resonance imaging with angiogram (MRI/MR-A). Conclusion: A lack of specific neurologic symptoms on admission urges the need for a dedicated imaging pathway for severely injured patients, reliable for the detection of cervical artery dissections. Although our modified CT protocol with mandatory dedicated CT-A led to false positives requiring additional magnetic resonance imaging, it likely helped reduce possible therapeutic delays.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Incidence and outcome of cervical artery dissection: a population-based study.
- Record: found
- Abstract: found
- Article: not found
Blunt carotid injury. Importance of early diagnosis and anticoagulant therapy.
- Record: found
- Abstract: found
- Article: not found