- Record: found
- Abstract: found
- Article: found
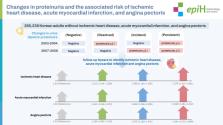
Changes in proteinuria and the associated risks of ischemic heart disease, acute myocardial infarction, and angina pectoris in Korean population
Read this article at
Abstract
OBJECTIVES
Proteinuria is widely used to predict cardiovascular risk. However, there is insufficient evidence to predict how changes in proteinuria may affect the incidence of cardiovascular disease.
METHODS
The study included 265,236 Korean adults who underwent health checkups in 2003-2004 and 2007-2008. They were categorized into 4 groups based on changes in proteinuria (negative: negative → negative; resolved: proteinuria ≥1+ → negative; incident: negative → proteinuria ≥1+; persistent: proteinuria ≥1+ → proteinuria ≥1+). We conducted 6 years of follow-up to identify the risks of developing ischemic heart disease (IHD), acute myocardial infarction (AMI), and angina pectoris according to changes in proteinuria. A multivariate Cox proportional-hazards model was used to calculate adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for incident IHD, AMI, and angina pectoris.
RESULTS
The IHD risk (expressed as HR [95% CI]) was the highest for persistent proteinuria, followed in descending order by incident and resolved proteinuria, compared with negative proteinuria (negative: reference, resolved: 1.211 [95% CI, 1.104 to 1.329], incident: 1.288 [95% CI, 1.184 to 1.400], and persistent: 1.578 [95% CI, 1.324 to 1.881]). The same pattern was associated with AMI (negative: reference, resolved: 1.401 [95% CI, 1.048 to 1.872], incident: 1.606 [95% CI, 1.268 to 2.035], and persistent: 2.069 [95% CI, 1.281 to 3.342]) and angina pectoris (negative: reference, resolved: 1.184 [95% CI, 1.065 to 1.316], incident: 1.275 [95% CI, 1.160 to 1.401], and persistent: 1.554 [95% CI, 1.272 to 1.899]).
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis.
- Record: found
- Abstract: not found
- Article: not found