- Record: found
- Abstract: found
- Article: found
Association between averaged intraoperative nociceptive response index and postoperative complications after lung resection surgery
Read this article at
Abstract
OBJECTIVES
Since postoperative complications, defined as Clavien–Dindo grade ≥II, correlate with long-term survival after lung resection surgery in patients with primary lung cancer, identification of intraoperative risk factors for postoperative complications is crucial for better perioperative management. In the present study, we investigated the possible association between intraoperative variables for use in anaesthetic management and Clavien–Dindo grade ≥II.
METHODS
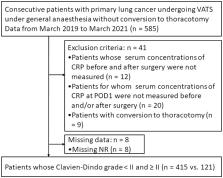
In this multi-institutional observational study, consecutive adult patients undergoing video-assisted thoracic surgery for primary lung cancer under general anaesthesia from March 2019 to April 2021 were enrolled. All patients were divided into 2 groups with Clavien–Dindo grade <II and ≥II. Uni- and multivariable analyses were performed to identify intraoperative risk factors.
RESULTS
After univariable analysis between patients with Clavien–Dindo grade <II ( n = 415) and ≥II ( n = 121), multivariable analysis revealed higher averaged nociceptive response (NR) index during surgery (mean NR), male sex, lower body mass index, longer duration of surgery, higher blood loss and lower urine volume, as independent risk factors for postoperative complications. In sensitivity analysis, based on the cut-off value of mean NR for postoperative complications, all patients were divided into high and low mean NR groups. The incidence of postoperative complications was significantly higher in patients with high mean NR ( n = 332) than in patients with low mean NR ( n = 204; P < 0.001).
Abstract
A higher incidence of postoperative complications after lung cancer surgery correlates with worse prognosis, including cancer recurrence and mortality [1–3].
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey.
- Record: found
- Abstract: not found
- Article: not found
Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial
- Record: found
- Abstract: found
- Article: not found
