- Record: found
- Abstract: found
- Article: found
Excessive Sleepiness and Longer Nighttime in Bed Increase the Risk of Cognitive Decline in Frail Elderly Subjects: The MAPT-Sleep Study
Read this article at
Abstract
Objective: To identify self-reported sleep-wake disturbances that increase the risk of cognitive decline over 1-year follow-up in frail participants.
Background: Risk factors for cognitive impairment need to be better identified especially at earliest stages of the pathogenesis. Sleep-wake disturbances may be critical factors to consider and were thus being assessed in this at-risk population for cognitive decline.
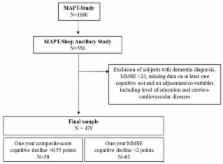
Methods: Frail elderly participants aged ≥70 years were selected from a subsample of the Multi-domain Alzheimer Preventive Trial (MAPT) for a sleep assessment (MAPT-sleep study) at 18-month follow-up (M18). Sleep-wake disturbances were evaluated using a clinical interview (duration of daytime and nighttime sleep, time in bed, number of naps, and presence of clinically-defined sleep disorders) and numerous validated questionnaires [Epworth Sleepiness Scale for excessive daytime sleepiness (EDS), Insomnia Severity Scale and Berlin Questionnaire]. Cognitive decline was defined as a difference between the MMSE and cognitive composite scores at M24 and M36 that was ranked in the lowest decile. Multivariate logistic regression models adjusted for several potential confounding factors were performed.
Results: Among the 479 frail participants, 63 developed MMSE-cognitive decline and 50 cognitive composite score decrease between M24 and M36. Subjects with EDS had an increased risk of MMSE decline (OR = 2.46; 95% CI [1.28; 4.71], p = 0.007). A longer time spent in bed during night was associated with cognitive composite score decline (OR = 1.32 [1.03; 1.71], p = 0.03). These associations persisted when controlling for potential confounders. Patients with MMSE score decline and EDS had more naps, clinically-defined REM-sleep Behavior Disorder, fatigue and insomnia symptoms, while patients with cognitive composite score decline with longer time in bed had increased 24-h total sleep time duration but with higher wake time after onset.
Conclusions: The risk of cognitive decline is higher in frailty subjects with EDS and longer nighttime in bed. Early detection of sleep-wake disturbances might help identifying frail subjects at risk of cognitive decline to further propose sleep health strategies to prevent cognitive impairment.
http://www.clinicaltrials.gov NCT00672685; Date of registration May, 2nd 2008.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
What sleep characteristics predict cognitive decline in the elderly?
- Record: found
- Abstract: found
- Article: not found
The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women.
- Record: found
- Abstract: found
- Article: found