- Record: found
- Abstract: found
- Article: found
Posterior Urethral Strictures
Read this article at
Abstract
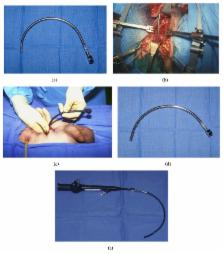
Pelvic fracture urethral injuries are typically partial and more often complete disruptions of the most proximal bulbar and distal membranous urethra. Emergency management includes suprapubic tube placement. Subsequent primary realignment to place a urethral catheter remains a controversial topic, but what is not controversial is that when there is the development of a stricture (which is usually obliterative with a distraction defect) after suprapubic tube placement or urethral catheter removal, the standard of care is delayed urethral reconstruction with excision and primary anastomosis. This paper reviews the management of patients who suffer pelvic fracture urethral injuries and the techniques of preoperative urethral imaging and subsequent posterior urethroplasty.
Related collections
Most cited references43
- Record: found
- Abstract: found
- Article: not found
Non-transecting anastomotic bulbar urethroplasty: a preliminary report.
- Record: found
- Abstract: found
- Article: not found
Urethral reconstruction for traumatic posterior urethral disruption: outcomes of a 25-year experience.
- Record: found
- Abstract: found
- Article: not found