- Record: found
- Abstract: found
- Article: found
Patterns of Multimorbidity and Differences in Healthcare Utilization and Complexity Among Acutely Hospitalized Medical Patients (≥65 Years) – A Latent Class Approach
Read this article at
Abstract
Purpose
The majority of acutely admitted older medical patients are multimorbid, receive multiple drugs, and experience a complex treatment regime. To be able to optimize treatment and care, we need more knowledge of the association between different patterns of multimorbidity and healthcare utilization and the complexity thereof. The purpose was therefore to investigate patterns of multimorbidity in a Danish national cohort of acutely hospitalized medical patients aged 65 and older and to determine the association between these multimorbid patterns with the healthcare utilization and complexity.
Patients and Methods
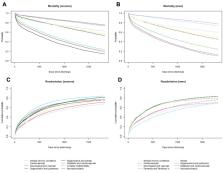
Longitudinal cohort study of 129,900 (53% women) patients. Latent class analysis (LCA) was used to develop patterns of multimorbidity based on 22 chronic conditions ascertained from Danish national registers. A latent class regression was used to test for differences in healthcare utilization and healthcare complexity among the patterns measured in the year leading up to the index admission.
Results
LCA identified eight distinct multimorbid patterns. Patients belonging to multimorbid patterns including the major chronic conditions; diabetes and chronic obstructive pulmonary disease was associated with higher odds of healthcare utilization and complexity than the reference pattern (“Minimal chronic conditions”). The pattern with the highest number of chronic conditions did not show the highest healthcare utilization nor complexity.
Conclusion
Our study showed that chronic conditions cluster together and that these patterns differ in healthcare utilization and complexity. Patterns of multimorbidity have the potential to be used in epidemiological studies of healthcare planning but should be confirmed in other population-based studies.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Recovery of activities of daily living in older adults after hospitalization for acute medical illness.
- Record: found
- Abstract: found
- Article: not found
