- Record: found
- Abstract: found
- Article: found
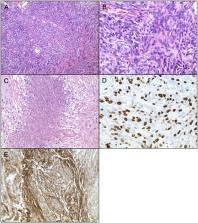
Review of Atypical and Anaplastic Meningiomas: Classification, Molecular Biology, and Management
Read this article at
Abstract
Although the majority of meningiomas are slow-growing and benign, atypical and anaplastic meningiomas behave aggressively with a penchant for recurrence. Standard of care includes surgical resection followed by adjuvant radiation in anaplastic and partially resected atypical meningiomas; however, the role of adjuvant radiation for incompletely resected atypical meningiomas remains debated. Despite maximum treatment, atypical, and anaplastic meningiomas have a strong proclivity for recurrence. Accumulating mutations over time, recurrent tumors behave more aggressively and often become refractory or no longer amenable to further surgical resection or radiation. Chemotherapy and other medical therapies are available as salvage treatment once standard options are exhausted; however, efficacy of these agents remains limited. This review discusses the risk factors, classification, and molecular biology of meningiomas as well as the current management strategies, novel therapeutic approaches, and future directions for managing atypical and anaplastic meningiomas.
Related collections
Most cited references152
- Record: found
- Abstract: found
- Article: found
The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary.
- Record: found
- Abstract: found
- Article: not found
The 2007 WHO Classification of Tumours of the Central Nervous System
- Record: found
- Abstract: found
- Article: not found