- Record: found
- Abstract: found
- Article: found
c-Met and PD-L1 on Circulating Exosomes as Diagnostic and Prognostic Markers for Pancreatic Cancer
Read this article at
Abstract
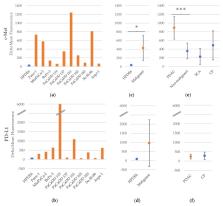
Exosomes are membrane vesicles which offer potential as blood derived biomarkers for malign tumors in clinical practice. Pancreatic cancer is counted among cancer diseases with the highest mortality. The present work seeks to assess whether pancreatic carcinomas release exosomes which express c-Met (proto-oncogene mesenchymal-epithelial transition factor) and PD-L1 (programmed cell death 1 ligand 1), and whether the detection of such expression in serum has diagnostic or prognostic meaning for the affected patients. Exosome isolation was performed on culture media of one benign pancreatic cell line and ten pancreatic carcinoma cell lines as well as on serum samples from 55 patients with pancreatic ductal adenocarcinoma (PDAC), 26 patients with chronic pancreatitis and 10 patients with benign serous cyst adenoma of the pancreas. Exosomes were bound to latex beads and stained with antibodies against c-Met or PD-L1. Analysis of fluorescence intensity was performed by flow cytometry. In terms of c-Met, the mean fluorescence intensity of PDAC-patients was significantly higher than the fluorescence intensity of the comparative patients with benign disease ( p < 0.001). A diagnostic test based on c-Met resulted in a sensitivity of 70%, a specificity of 85% and a diagnostic odds ratio of 13:2. The specificity of the test can be further improved by combining it with the established tumor marker carbohydrate antigen 19-9 (CA 19-9). In addition, c-Met-positive patients showed a significantly shorter postoperative survival time (9.5 vs. 21.7 months, p < 0.001). In terms of PD-L1, no significant difference between fluorescence intensity of PDAC-patients and comparative patients was detectable. However, PD-L1-positive PDAC-patients also showed a significantly shorter postoperative survival time (7.8 vs. 17.2 months, p = 0.043). Thus, both markers can be considered as negative prognostic factors.
Related collections
Most cited references13

- Record: found
- Abstract: found
- Article: found
PD-L1 expression in human cancers and its association with clinical outcomes
- Record: found
- Abstract: found
- Article: not found
The clinical utility of CA 19-9 in pancreatic adenocarcinoma: diagnostic and prognostic updates.
- Record: found
- Abstract: found
- Article: not found