- Record: found
- Abstract: found
- Article: found
Pirfenidone attenuates bleomycin-induced pulmonary fibrosis in mice by regulating Nrf2/Bach1 equilibrium
Read this article at
Abstract
Background
Oxidative stress is one of the important factors involved in the pathogenesis of idiopathic pulmonary fibrosis (IPF). The equilibrium of Nuclear factor-erythroid-related factor 2 (Nrf2)/[BTB (broad-complex, tramtrack and bric-a-brac) and CNC (cap‘n’collar protein) homology 1, Bach1] determines the expression level of antioxidant factors, further regulating the function of oxidation/antioxidation capacity. Pirfenidone (PFD) is one of two currently for IPF therapy approved drugs. PFD regulates intracellular antioxidants, inhibits secretion of inflammatory cytokines and collagen synthesis. However the mechanisms of its antioxidant effects remain elusive.
Methods
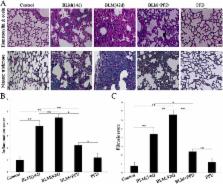
Effects of PFD treatment were studied in mouse lung fibroblasts (MLF) following induction by transforming-growth factor beta 1 (TGF-β1) and in mice following bleomycin-induced lung fibrosis. The mRNA and protein levels of oxidative stress-related factors Nrf2/Bach1 and their downstream antioxidant factors heme oxygenase-1 (Ho-1) and glutathione peroxidase 1 (Gpx1) were determined by RT-PCR and Western blot. Fibrosis-related cytokines interleukin-6 (IL-6) and myofibroblast markers type 1 collagen α1 (COL1A1) levels in supernate of MLF, serum, and bronchoalveolar lavage fluid (BALF) as well as malondialdehyde (MDA) in serum and BALF were detected by ELISA, reactive oxygen species (ROS) generation was measured by 2′,7′- dichlorofluorescin diacetate (DCFH-DA) assay and lung pathological/morphological alterations in mice were observed by HE and Masson to assess the antioxidant mechanism and therapeutic effects on pulmonary fibrosis induced by bleomycin.
Results
PFD inhibited Bach1 mRNA and protein expressions in mouse lung fibroblasts induced by TGF-β1 and lung tissues with pulmonary fibrosis induced by bleomycin. Furthermore, it improved Nrf2, Ho-1 and Gpx1 mRNA and protein expressions. After PFD treatment, COL1A1and IL-6 levels in supernate of MLF, serum, and BALF as well as ROS in lung tissues and MDA in serum and BALF from a mouse with pulmonary fibrosis were significantly decreased, and the infiltration of lung inflammatory cells and fibrosis degree were alleviated.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Simple method of estimating severity of pulmonary fibrosis on a numerical scale.
- Record: found
- Abstract: found
- Article: not found
A transcriptional co-repressor that interacts with nuclear hormone receptors.
- Record: found
- Abstract: found
- Article: not found