- Record: found
- Abstract: found
- Article: found
TRP Channels in the Focus of Trigeminal Nociceptor Sensitization Contributing to Primary Headaches
Read this article at
Abstract
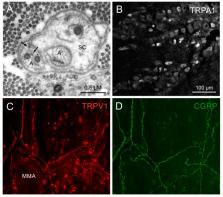
Pain in trigeminal areas is driven by nociceptive trigeminal afferents. Transduction molecules, among them the nonspecific cation channels transient receptor potential vanilloid 1 (TRPV1) and ankyrin 1 (TRPA1), which are activated by endogenous and exogenous ligands, are expressed by a significant population of trigeminal nociceptors innervating meningeal tissues. Many of these nociceptors also contain vasoactive neuropeptides such as calcitonin gene-related peptide (CGRP) and substance P. Release of neuropeptides and other functional properties are frequently examined using the cell bodies of trigeminal neurons as models of their sensory endings. Pathophysiological conditions cause phosphorylation, increased expression and trafficking of transient receptor potential (TRP) channels, neuropeptides and other mediators, which accelerate activation of nociceptive pathways. Since nociceptor activation may be a significant pathophysiological mechanism involved in both peripheral and central sensitization of the trigeminal nociceptive pathway, its contribution to the pathophysiology of primary headaches is more than likely. Metabolic disorders and medication-induced painful states are frequently associated with TRP receptor activation and may increase the risk for primary headaches.
Related collections
Most cited references149
- Record: found
- Abstract: found
- Article: not found
Pathophysiology of Migraine: A Disorder of Sensory Processing.
- Record: found
- Abstract: found
- Article: not found
The menthol receptor TRPM8 is the principal detector of environmental cold.
- Record: found
- Abstract: found
- Article: not found