- Record: found
- Abstract: found
- Article: found
Mycobactericidal Effects of Different Regimens Measured by Molecular Bacterial Load Assay among People Treated for Multidrug-Resistant Tuberculosis in Tanzania
Read this article at
Abstract
Rifampin or multidrug-resistant tuberculosis (RR/MDR-TB) treatment has largely transitioned to regimens free of the injectable aminoglycoside component, despite the drug class’ purported bactericidal activity early in treatment. We tested whether Mycobacterium tuberculosis
ABSTRACT
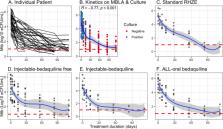
Rifampin or multidrug-resistant tuberculosis (RR/MDR-TB) treatment has largely transitioned to regimens free of the injectable aminoglycoside component, despite the drug class’ purported bactericidal activity early in treatment. We tested whether Mycobacterium tuberculosis killing rates measured by tuberculosis molecular bacterial load assay (TB-MBLA) in sputa correlate with composition of the RR/MDR-TB regimen. Serial sputa were collected from patients with RR/MDR- and drug-sensitive TB at days 0, 3, 7, and 14, and then monthly for 4 months of anti-TB treatment. TB-MBLA was used to quantify viable M. tuberculosis 16S rRNA in sputum for estimation of colony forming units per ml (eCFU/ml). M. tuberculosis killing rates were compared among regimens using nonlinear-mixed-effects modeling of repeated measures. Thirty-seven patients produced 296 serial sputa and received treatment as follows: 13 patients received an injectable bedaquiline-free reference regimen, 9 received an injectable bedaquiline-containing regimen, 8 received an all-oral bedaquiline-based regimen, and 7 patients were treated for drug-sensitive TB with conventional rifampin/isoniazid/pyrazinamide/ethambutol (RHZE). Compared to the adjusted M. tuberculosis killing of −0.17 (95% confidence interval [CI] −0.23 to −0.12) for the injectable bedaquiline-free reference regimen, the killing rates were −0.62 (95% CI −1.05 to −0.20) log 10 eCFU/ml for the injectable bedaquiline-containing regimen ( P = 0.019), −0.35 (95% CI −0.65 to −0.13) log 10 eCFU/ml for the all-oral bedaquiline-based regimen ( P = 0.054), and −0.29 (95% CI −0.78 to +0.22) log 10 eCFU/ml for the RHZE regimen ( P = 0.332). Thus, M. tuberculosis killing rates from sputa were higher among patients who received bedaquiline but were further improved with the addition of an injectable aminoglycoside.
Related collections
Most cited references50
- Record: found
- Abstract: found
- Article: not found
Treatment correlates of successful outcomes in pulmonary multidrug-resistant tuberculosis: an individual patient data meta-analysis
- Record: found
- Abstract: found
- Article: not found
Aminoglycosides: An Overview.
- Record: found
- Abstract: found
- Article: found