- Record: found
- Abstract: found
- Article: found
Effect of ticagrelor on the serum level of hs-CRP, ESM-1 and short-term prognosis of patients with acute STEMI
Read this article at
Abstract
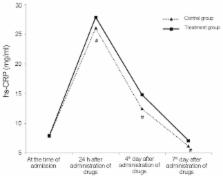
The aim of the present study was to observe and investigate the changes in the serum level of high-sensitivity C-reactive protein (hs-CRP), the endothelial cell-specific molecule-1 (ESM-1) and short-term prognosis of patients with ST-segment elevation myocardial infarction (STEMI) treated by ticagrelor. We enrolled 107 patients with acute STEMI who were admitted in the Department of Cardiology for the first time with occurrence of symptoms, and we successfully performed emergency operation of percutaneous coronary intervention. The patients were divided into two groups, 54 patients in the ticagrelor group (treatment group) and 53 patients in the clopidogrel group (control group), according to the administration of ticagrelor or clopidogrel in dual anti-platelet therapy. Then, we observed the changes at the time of admission, at 24 h, and 4th and 7th day after administration and investigated the correlations between them and the effect of ticagrelor on the short-term prognosis of acute STEMI patients. Significant increases of the serum levels of hs-CRP and ESM-1 were seen in patients of the two groups 24 h after administration of drugs with statistically significant differences between the groups (P<0.05), and on the 4th and 7th day we found a downward trend with statistically significant differences (P<0.05). The level of ESM-1 enhanced the increase of hs-CRP, indicating there was a positive correlation between ESM-1 and hs-CRP (r=0.535, P<0.001). A comparison of the occurrence rates of ischemic outcome event, bleeding and overall adverse events between the two groups yielded no statistically significant difference (P>0.05). In conclusion, the present study demonstrates that ticagrelor can reduce the prevalence of inflammatory reactions rapidly and stabilize the functions of vascular endothelium to improve the stability of atherosclerosis plaque and decrease the occurrence rate of thrombosis as well as ischemic outcome event without any obvious increase in the risk of bleeding. Thus, ticagrelor should be recommended in clinical practices for the treatment of patients with STEMI.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction.
- Record: found
- Abstract: found
- Article: not found

