- Record: found
- Abstract: found
- Article: found
Evaluation of a programme for ‘Rapid Assessment of Febrile Travelers’ (RAFT): a clinic-based quality improvement initiative
Read this article at
Abstract
Background
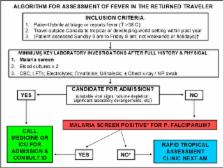
Fever in the returned traveller is a potential medical emergency warranting prompt attention to exclude life-threatening illnesses. However, prolonged evaluation in the emergency department (ED) may not be required for all patients. As a quality improvement initiative, we implemented an algorithm for rapid assessment of febrile travelers (RAFT) in an ambulatory setting.
Methods
Criteria for RAFT referral include: presentation to the ED, reported fever and travel to the tropics or subtropics within the past year. Exclusion criteria include Plasmodium falciparum malaria, and fulfilment of admission criteria such as unstable vital signs or significant laboratory derangements. We performed a time series analysis preimplementation and postimplementation, with primary outcome of wait time to tropical medicine consultation. Secondary outcomes included number of ED visits averted for repeat malaria testing, and algorithm adherence.
Results
From February 2014 to December 2015, 154 patients were seen in the RAFT clinic: 68 men and 86 women. Median age was 36 years (range 16–78 years). Mean time to RAFT clinic assessment was 1.2±0.07 days (range 0–4 days) postimplementation, compared to 5.4±1.8 days (range 0–26 days) prior to implementation (p<0.0001). The RAFT clinic averted 132 repeat malaria screens in the ED over the study period (average 6 per month). Common diagnoses were: traveller's diarrhoea (n=27, 17.5%), dengue (n=12, 8%), viral upper respiratory tract infection (n=11, 7%), chikungunya (n=10, 6.5%), laboratory-confirmed influenza (n=8, 5%) and lobar pneumonia (n=8, 5%).
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
Fever in returned travelers: results from the GeoSentinel Surveillance Network.
- Record: found
- Abstract: found
- Article: not found
Spectrum of enteropathogens detected by the FilmArray GI Panel in a multicentre study of community-acquired gastroenteritis.
- Record: found
- Abstract: found
- Article: not found