- Record: found
- Abstract: found
- Article: found
Using mHealth to Increase the Reach of Local Guidance to Health Professionals as Part of an Institutional Response Plan to the COVID-19 Outbreak: Usage Analysis Study
Abstract
Background
The ongoing coronavirus disease (COVID-19) pandemic forced health jurisdictions worldwide to significantly restructure and reorganize their medical activities. In response to the rapidly evolving body of evidence, a solid communication strategy is needed to increase the reach of and adherence to locally drafted and validated guidance to aide medical staff with COVID-19–related clinical decisions.
Objective
We present a usage analysis of a dedicated mobile health (mHealth) platform as part of an institutional knowledge dissemination strategy of COVID-19–related guidance to all health care workers (HCWs) in a large academic hospital.
Methods
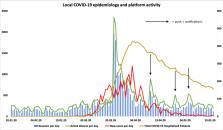
A multidisciplinary team of experts drafted local guidance related to COVID-19. In total, 60 documents and 17 external links were made available through the platform. Documents were disseminated using a recently deployed mHealth platform for HCWs. Targeted dissemination of COVID-19–related content began on March 22, 2020. Using a third-party statistics tool, data concerning user activity and content use was anonymously collected. A quantitative analysis of user activity was performed over a 4-month period, separated into 3 periods: 2 months before (Period A), 2 weeks after (Period B), and 6 weeks following (Period C) targeted dissemination. Regional epidemiological data (daily new COVID-19 cases and total COVID-19–related hospitalizations) was extracted from an official registry.
Results
During the study period, the platform was downloaded by 1233 new users. Consequently, the total number of users increased from 1766 users before Period A to a total of 2999 users at the end of Period C. We observed 27,046 document views, of which 12,728 (47.1%) were COVID-19–related. The highest increase in activity occurred in Period B, rapidly following targeted dissemination, with 7740 COVID-19–related content views, representing 71.2% of total content views within the abovementioned period and 550 daily views of COVID-19–related documents. Total documents consulted per day increased from 117 (IQR 74-160) to 657 (IQR 481-1051), P<.001. This increase in activity followed the epidemiological curbing of newly diagnosed COVID-19 cases, which peaked during Period B. Total active devices doubled from 684 to 1400, daily user activity increased fourfold, and the number of active devices rose from 53 (IQR 40-70) to 210 (IQR 167-297), P<.001. In addition, the number of sessions per day rose from 166 (IQR 110-246) to 704 (IQR 517-1028), P<.001. A persistent but reduced increase in total documents consulted per day (172 [IQR 131-251] versus 117 [IQR 74-160], P<.001) and active devices (71 [IQR 64-89] versus 53 [IQR 40-70]) was observed in Period C compared to Period A, while only 29.8% of the content accessed was COVID-19–related. After targeted dissemination, an immediate increase in activity was observed after push notifications were sent to users.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: found
World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19)
- Record: found
- Abstract: found
- Article: not found
COVID-19: protecting health-care workers
- Record: found
- Abstract: found
- Article: not found