- Record: found
- Abstract: found
- Article: found
Establishment of reference values of the caudal vena cava by fast‐ultrasonography through different views in healthy dogs
Read this article at
Abstract
Background
Clinical assessment of intravascular volume status is challenging. In humans, ultrasonographic assessment of the inferior vena cava diameter, directly or as a ratio to the aortic diameter is used to estimate intravascular volume status.
Objectives
To ultrasonographically obtain reference values (RV) for caudal vena cava diameter (CVC D), area (CVC a) and aortic ratios using 3 views in awake healthy dogs.
Methods
Prospective, multicenter, observational study. Two observer pairs evaluated CVC D by a longitudinal subxiphoid view (SV), a transverse 11th‐13th right hepatic intercostal view (HV), and a longitudinal right paralumbar view (PV). Inter‐rater agreements were estimated using concordance correlation coefficients (CCC). For body weight (BW) ‐dependent variables, RVs were calculated using allometric scaling for variables with a CCC ≥ 0.7.
Results
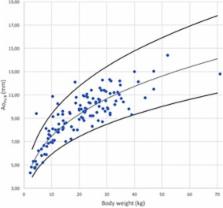
The CCC was ≤0.43 for the CVC/aorta ratio at the PV and ≤0.43 in both inspiration and expiration for CVC at the SV. The RVs using allometric scaling for CVC a at the HV for inspiration, expiration, and for CVC D at the PV were 6.16 × BW 0.762, 7.24 × BW 0.787, 2.79 × BW 0.390, respectively.
Conclusions and Clinical Importance
The CVC D, measured at the HV and PV in healthy awake dogs of various breeds has good inter‐rater agreement suggesting these sites are reliable in measuring CVC D. Established RVs for CVC D for these sites need further comparison to results obtained in hypovolemic and hypervolemic dogs to determine their usefulness to evaluate volume status in dogs.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
A concordance correlation coefficient to evaluate reproducibility.
- Record: found
- Abstract: found
- Article: not found
Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares.
- Record: found
- Abstract: found
- Article: not found