- Record: found
- Abstract: found
- Article: found
Cerebral aneurysm treatment: modern neurovascular techniques
review-article
25 October 2016
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
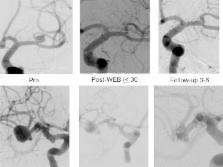
Endovascular treatment of cerebral aneurysm continues to evolve with the development of new technologies. This review provides an overview of the recent major innovations in the neurointerventional space in recent years.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment.
David O Wiebers, J P Whisnant, J. Huston … (2003)
- Record: found
- Abstract: found
- Article: not found
Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial.
Tibor Becske, David F Kallmes, Işil Saatçi … (2013)
- Record: found
- Abstract: found
- Article: not found
Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils.
Jean Raymond, François Guilbert, Alain Weill … (2003)