- Record: found
- Abstract: found
- Article: found
Synthetic surfactant containing SP-B and SP-C mimics is superior to single-peptide formulations in rabbits with chemical acute lung injury
Read this article at
Abstract
Background. Chemical spills are on the rise and inhalation of toxic chemicals may induce chemical acute lung injury (ALI)/acute respiratory distress syndrome (ARDS). Although the pathophysiology of ALI/ARDS is well understood, the absence of specific antidotes has limited the effectiveness of therapeutic interventions.
Objectives. Surfactant inactivation and formation of free radicals are important pathways in (chemical) ALI. We tested the potential of lipid mixtures with advanced surfactant protein B and C (SP-B and C) mimics to improve oxygenation and lung compliance in rabbits with lavage- and chemical-induced ALI/ARDS.
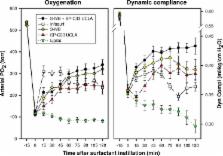
Methods. Ventilated young adult rabbits underwent repeated saline lung lavages or underwent intratracheal instillation of hydrochloric acid to induce ALI/ARDS. After establishment of respiratory failure rabbits were treated with a single intratracheal dose of 100 mg/kg of synthetic surfactant composed of 3% Super Mini-B (S-MB), a SP-B mimic, and/or SP-C33 UCLA, a SP-C mimic, in a lipid mixture (DPPC:POPC:POPG 5:3:2 by weight), the clinical surfactant Infasurf ®, a bovine lung lavage extract with SP-B and C, or synthetic lipids alone. End-points consisted of arterial oxygenation, dynamic lung compliance, and protein and lipid content in bronchoalveolar lavage fluid. Potential mechanism of surfactant action for S-MB and SP-C33 UCLA were investigated with captive bubble surfactometry (CBS) assays.
Results. All three surfactant peptide/lipid mixtures and Infasurf equally lowered the minimum surface tension on CBS, and also improved oxygenation and lung compliance. In both animal models, the two-peptide synthetic surfactant with S-MB and SP-C33 UCLA led to better arterial oxygenation and lung compliance than single peptide synthetic surfactants and Infasurf. Synthetic surfactants and Infasurf improved lung function further in lavage- than in chemical-induced respiratory failure, with the difference probably due to greater capillary-alveolar protein leakage and surfactant dysfunction after HCl instillation than following lung lavage. At the end of the duration of the experiments, synthetic surfactants provided more clinical stability in ALI/ARDS than Infasurf, and the protein content of bronchoalveolar lavage fluid was lowest for the two-peptide synthetic surfactant with S-MB and SP-C33 UCLA.
Conclusion. Advanced synthetic surfactant with robust SP-B and SP-C mimics is better equipped to tackle surfactant inactivation in chemical ALI than synthetic surfactant with only a single surfactant peptide or animal-derived surfactant.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
Surfactant replacement therapy for preterm and term neonates with respiratory distress.
- Record: found
- Abstract: found
- Article: not found
Effect of exogenous surfactant (calfactant) in pediatric acute lung injury: a randomized controlled trial.
- Record: found
- Abstract: found
- Article: not found