- Record: found
- Abstract: found
- Article: found
Cardiorespiratory responses to 6-minute walk test in interstitial lung disease: not always a submaximal test
Read this article at
Abstract
Background
The 6-minute walk test (6MWT) is used to measure exercise capacity and assess prognosis in interstitial lung disease (ILD). Although the 6MWT is usually considered to be a test of submaximal exercise capacity in ILD, the physiological load imposed by this test is not well described and 6MWT outcomes are poorly understood. This study aimed to compare cardiorespiratory responses to 6MWT and cardiopulmonary exercise test (CPET) in people with ILD.
Methods
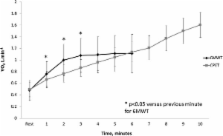
47 participants with ILD (27 idiopathic pulmonary fibrosis (IPF), mean age 71 (SD 12) years, diffusing capacity for carbon monoxide (TLCO) 49(15) %predicted) undertook CPET and 6MWT on the same day in random order. Oxygen uptake (VO 2), ventilation (VE) and carbon dioxide production (VCO 2) were assessed during each test using a portable metabolic cart.
Results
The VO 2peak during the 6MWT was lower than during CPET (1.17(0.27) vs 1.30(0.37) L.min −1, p = 0.001), representing an average of 94% (range 62-135%) of CPET VO 2peak. Achieving a higher percentage of CPET VO 2peak on 6MWT was associated with lower TLCO %predicted (r = −0.43, p = 0.003) and more desaturation during walking (r = −0.46, p = 0.01). The VEpeak and VCO 2peak were significantly lower during 6MWT than CPET (p < 0.05). However, participants desaturated more during the 6MWT (86(6)% vs 89(4)%, p < 0.001). The degree of desaturation was not affected by the percent of peak VO 2 achieved during the 6MWT. Responses were similar in the subgroup with IPF.
Conclusions
On average, the 6MWT elicits a high but submaximal oxygen uptake in people with ILD. However the physiological load varies between individuals, with higher peak VO 2 in those with more severe disease that may match or exceed that achieved on CPET. The 6MWT is not always a test of submaximal exercise capacity in people with ILD.
Related collections
Most cited references24
- Record: found
- Abstract: not found
- Article: not found
Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society.
- Record: found
- Abstract: found
- Article: not found
Six-minute-walk test in idiopathic pulmonary fibrosis: test validation and minimal clinically important difference.
- Record: found
- Abstract: found
- Article: not found
