- Record: found
- Abstract: found
- Article: found
Endoscopic resection of acetabular screw tip to decompress sciatic nerve following total hip arthroplasty
Read this article at
Abstract
Background
Sciatic nerve injuries following total hip arthroplasty are disabling complications. Although degrees of injury are variable from neuropraxia to neurotmesis, mechanical irritation of sciatic nerve might be occurred by protruding hardware. This case shows endoscopic decompression for protruded acetabular screw irritating sciatic nerve, the techniques described herein may permit broader arthroscopic/endoscopic applications for management of complications after reconstructive hip surgery.
Case presentation
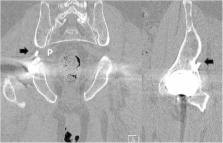
An 80-year-old man complained of severe pain and paresthesias following acetabular component revision surgery. Physical findings included right buttock pain with radiating pain to lower extremity. Radiographs and computed tomography imaging showed that the sharp end of protruded screw invaded greater sciatic foramen anterior to posterior and distal to proximal direction at sciatic notch level. A protruding tip of the acetabular screw at the sciatic notch was decompressed by use of techniques gained from experience performing endoscopic sciatic nerve decompression. The pre-operative pain and paresthesias resolved post-operatively after recovering from anesthesia.
Conclusions
This case report describes the first documented endoscopic resection of the tip of the acetabular screw irritating sciatic nerve after total hip arthroplasty. If endoscopic resection of an offending acetabular screw can be performed in a safe and minimally invasive manner, one can envision a future expansion of the role of hip arthroscopic surgery in several complications management after total hip arthroplasty.
Related collections
Most cited references7
- Record: found
- Abstract: found
- Article: not found
Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty.
- Record: found
- Abstract: found
- Article: not found
Update on nerve palsy associated with total hip replacement.
- Record: found
- Abstract: found
- Article: not found