- Record: found
- Abstract: found
- Article: found
Visceral artery pseudoaneurysms: two case reports and a review of the literature
Read this article at
Abstract
Background
Visceral artery pseudoaneurysms are relatively rare but have a high mortality rate in case of rupture. Their detection in the last decades is rising due to an increased use of computed tomography and angiography. However, due to the nonspecific nature of the clinical symptoms and signs, diagnosis is often delayed or missed. We describe two cases of patients presenting with nonspecific abdominal complaints and anemia leading to a diagnosis of visceral pseudoaneurysm. Both cases are successfully treated with a different endovascular intervention.
Case presentation
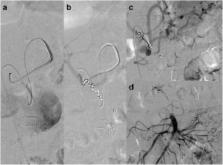
The first case is a 67-year-old Caucasian man presenting with diffuse abdominal pain, vomiting, diarrhea, and weight loss. Digital angiography showed a complex pseudoaneurysm of the superior mesenteric artery. The patient was treated with stent placement and selective embolization of the afferent branches.
The second patient is a 78-year-old Caucasian man with a history of chronic pancreatitis admitted with epigastric pain, rectal bleeding and melena. Angiography showed a pseudoaneurysm of the gastroduodenal artery. The patient was successfully treated with coil embolization.
Conclusions
We report two cases of visceral pseudoaneurysms and review the literature concerning etiology, presentation, diagnosis, and treatment.
Visceral artery pseudoaneurysms should be considered in the differential diagnosis of a patient with nonspecific abdominal symptoms. Diagnosis is often made with computed tomography or computed tomography angiography but digital angiography remains the gold standard. Treatment options include surgical, endovascular or percutaneous interventions. The choice of treatment is case specific.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Pseudoaneurysms and the role of minimally invasive techniques in their management.
- Record: found
- Abstract: found
- Article: not found
Surgical treatment of visceral artery aneurysms: A 25-year experience.
- Record: found
- Abstract: found
- Article: not found