- Record: found
- Abstract: found
- Article: not found
The Impact of Maternal Obesity and Gestational Weight Gain on Early and Mid-Pregnancy Lipid Profiles
Abstract
Objective
We evaluated the impact of maternal overweight/obesity and excessive weight gain on maternal serum lipids in the first and second trimester of pregnancy.
Design and Methods
Prospective data were collected for 225 women. Maternal serum lipids and fatty acids were measured at <13 weeks and between 24–28 weeks. Analyses were stratified by normal weight versus overweight/obese status and excessive vs. non-excessive weight gain.
Results
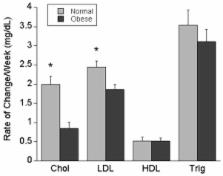
Overweight/obese women had higher baseline cholesterol (161.3±29.6 vs 149.4±26.8 mg/dL, p<0.01), LDL (80.0±19.9 vs 72.9 ±18.8 mg/dL, p<0.01) and triglycerides ( 81.7±47.2 vs 69.7±40.3 mg/dL, p=0.05) when compared to normal weight women, while HDL (43.6 ±10.4 47.6±11.5 mg/dL, p<0.01) was lower. However, cholesterol and LDL increased at a higher weekly rate in normal weight women, resulting in higher total cholesterol in normal weight women (184.1±28.1 vs. 176.0 ±32.1 mg/dL, p=0.05) at 24–28 weeks. Excessive weight gain did not affect the rate of change in lipid profiles in either group. Overweight/obese women had higher levels of arachidonic acid at both time points.
Related collections
Most cited references30
- Record: found
- Abstract: not found
- Article: not found
A rapid method of total lipid extraction and purification.
- Record: found
- Abstract: found
- Article: not found
A prospective study of pregravid determinants of gestational diabetes mellitus.
- Record: found
- Abstract: found
- Article: not found
